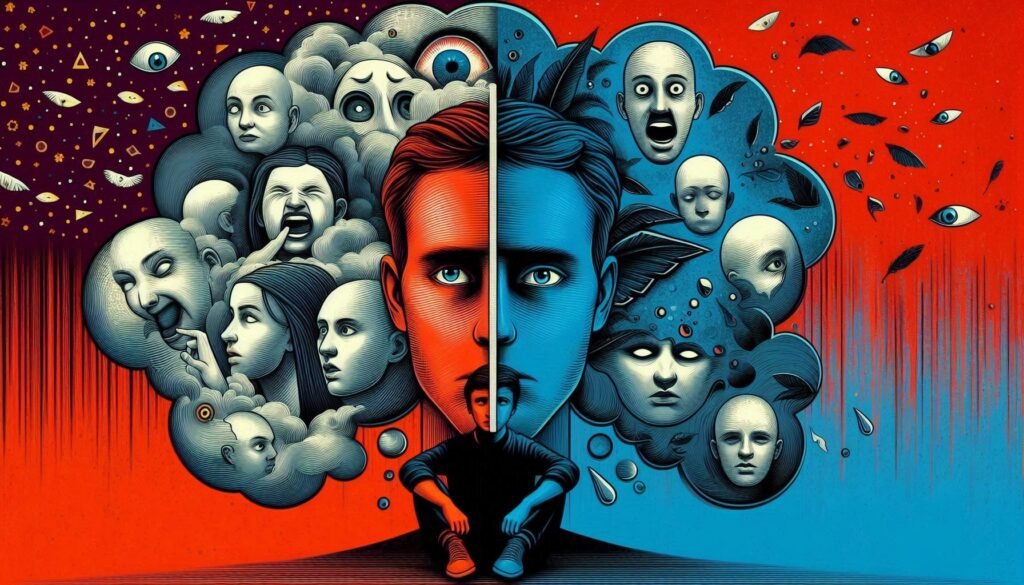
When we think about personality disorders, the term “odd” often comes to mind. This is especially true for Cluster A Personality Disorders, a group that encompasses Paranoid, Schizoid, and Schizotypal disorders. These conditions are characterized by unconventional behaviors and ways of thinking. Individuals with these disorders may seem peculiar or socially withdrawn, leading to misunderstandings in their personal relationships.
Understanding Cluster A Personality Disorders is crucial not only for mental health professionals but also for friends and family who wish to support their loved ones. This blog post will explore the nuances of these disorders—from diagnostic criteria to treatment options—providing insights into this fascinating yet complex area of psychology. Whether you’re seeking knowledge for personal reasons or simply expanding your understanding of human behavior, delve deeper as we uncover the layers behind these “odd” personalities.

Overview of Cluster A: Paranoid, Schizoid, and Schizotypal Personality Disorders
Cluster A Personality Disorders are categorized as “odd or eccentric” in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). This cluster includes three distinct disorders: Paranoid, Schizoid, and Schizotypal.
Paranoid Personality Disorder is marked by pervasive distrust and suspicion of others. Individuals often interpret benign remarks as threatening, leading to long-standing grievances.
Schizoid Personality Disorder involves a detachment from social relationships. Those affected may appear indifferent to social interactions and prefer solitary activities, showing little interest in forming emotional connections.
Schizotypal Personality Disorder combines elements of thought disorder with eccentric behavior. Individuals experience peculiar beliefs or magical thinking while maintaining basic reality testing. They may exhibit odd speech patterns or dress unusually.
These disorders share common traits but manifest uniquely within each individual, influencing their thoughts and behaviors significantly. Understanding these distinctions is essential for proper diagnosis and treatment strategies.
Common Characteristics and Distinguishing Features of Cluster A Disorders
Cluster A personality disorders are characterized by bizarre or eccentric behaviors. This cluster includes paranoid, schizoid, and schizotypal disorders, each with unique traits.
Individuals with paranoid personality disorder often exhibit deep-seated distrust and suspicion of others. They may interpret benign actions as threatening and hold grudges for long periods.
Those diagnosed with schizoid personality disorder display a detachment from social relationships. They tend to prefer solitary activities, showing limited emotional expression and little desire for intimacy.
Schizotypal personality disorder encompasses peculiarities in thought patterns and behavior. Individuals may experience odd beliefs or magical thinking, along with discomfort in close relationships. Their speech can be unusual or tangential.
These distinct features set Cluster A apart from other personality disorder categories while highlighting the challenges individuals face in social contexts. Understanding these characteristics is essential for accurate diagnosis and effective support strategies.
Prevalence and Demographics of Cluster A Personality Disorders
Cluster A Personality Disorders, which include paranoid, schizoid, and schizotypal traits, are relatively uncommon but significant in mental health discussions. Studies suggest that these disorders affect approximately 2% to 5% of the general population.
Demographically, these disorders appear across various age groups and genders. However, some research indicates a higher prevalence among males compared to females. Specifically, paranoid personality disorder is often more frequently diagnosed in men.
Cultural factors also play an essential role in how these disorders manifest. For instance, different societies may interpret eccentric behaviors uniquely. This can influence diagnostic rates and treatment approaches globally.
Age at onset varies as well; symptoms typically emerge during adolescence or early adulthood. Understanding this demographic landscape helps clinicians tailor their interventions effectively for individuals grappling with Cluster A traits.
Genetic and Environmental Risk Factors for Cluster A Disorders
Genetic and environmental factors play significant roles in the development of Cluster A Personality Disorders. Research suggests that these disorders may have a hereditary component, with family histories indicating higher prevalence among relatives. Genetic variations affecting neurotransmitter systems could contribute to their manifestation.
Environmental influences are equally important. Early childhood experiences, such as trauma or neglect, can shape personality development. Social isolation during formative years might also increase vulnerability to these disorders.
Stressful life events often exacerbate symptoms too. Individuals exposed to high levels of stress may find it challenging to cope with social situations, further entrenching their eccentric behaviors.
Understanding these risk factors is essential for early intervention and support strategies tailored for those affected by Cluster A Disorders. More research is needed to unravel the complexities of how genetics and environment intertwine in this context.
Neurocognitive Profiles Associated with Cluster A Personality Disorders
Cluster A personality disorders are often linked to unique neurocognitive profiles. Individuals with these disorders may show atypical brain functioning, particularly in regions associated with social cognition and emotional processing.
Research indicates that those with paranoid traits might exhibit heightened activity in the amygdala. This area is crucial for fear responses and might explain their suspicious nature.
On the other hand, individuals diagnosed with schizoid personality disorder tend to display reduced connectivity within networks responsible for social engagement. This could contribute to their preference for solitude and emotional detachment.
Schizotypal individuals often showcase cognitive distortions, such as magical thinking or odd beliefs. Neuroimaging studies reveal alterations in the prefrontal cortex, which could affect judgment and reality testing.
Understanding these neurocognitive differences can aid mental health professionals in tailoring effective interventions for those affected by Cluster A personality disorders.
The Relationship Between Cluster A Disorders and Schizophrenia Spectrum
Cluster A personality disorders are often viewed through the lens of their relationship with the schizophrenia spectrum. This connection is significant as both groups share traits that can influence diagnosis and treatment.
Individuals with paranoid, schizoid, or schizotypal personality disorders may display symptoms reminiscent of schizophrenia, such as social withdrawal or eccentric behavior. However, these individuals generally retain a clearer grasp on reality compared to those diagnosed with schizophrenia.
Schizotypal personality disorder is particularly noteworthy due to its overlap in symptoms like magical thinking and unusual perceptual experiences. These characteristics can blur diagnostic lines between Cluster A disorders and schizoaffective conditions.
Understanding this relationship helps mental health professionals refine their assessments. It also emphasizes the importance of comprehensive evaluations for effective intervention strategies tailored to each individual’s needs.
Impact on Social Functioning and Interpersonal Relationships
Cluster A personality disorders can significantly impair social functioning and interpersonal relationships. Individuals with these disorders often struggle to engage meaningfully with others.
People diagnosed with paranoid personality disorder may exhibit a pervasive distrust and suspicion of others, leading them to isolate themselves or misinterpret social cues. This can create barriers in forming close bonds.
Those with schizoid personality disorder typically prefer solitude over social interactions. Their emotional detachment makes it difficult for them to express feelings, leaving friends and family feeling disconnected or unvalued.
Schizotypal individuals often display eccentric thoughts and behaviors that may alienate peers. They might experience heightened anxiety in social settings, which further hinders their ability to develop healthy relationships.
These challenges contribute not only to loneliness but also exacerbate the symptoms of the disorders, creating a cycle that’s hard to break.
Diagnostic Criteria and Assessment Tools for Cluster A Disorders
Diagnostic criteria for Cluster A Personality Disorders are outlined in the DSM-5. This manual categorizes three specific disorders: Paranoid, Schizoid, and Schizotypal.
For each disorder, distinct traits must be present. For instance, individuals with Paranoid Personality Disorder often exhibit pervasive distrust and suspicion of others. Those diagnosed with Schizoid Personality Disorder typically show a detachment from social relationships and limited emotional expression. Meanwhile, Schizotypal Personality Disorder is characterized by eccentric behavior and cognitive distortions.
Assessment tools include structured interviews like the Structured Clinical Interview for DSM-5 (SCID). Self-report questionnaires can also provide insight into personality traits associated with these disorders.
Clinicians often utilize comprehensive assessments to evaluate an individual’s history and current functioning effectively. These methods help ensure accurate diagnosis and inform treatment planning tailored to each person’s unique needs.
Differential Diagnosis: Distinguishing Between Cluster A Disorders
Differentiating between Cluster A personality disorders—paranoid, schizoid, and schizotypal—can be challenging due to overlapping symptoms. Each disorder has unique traits that require careful consideration.
Paranoid personality disorder is characterized by a pervasive distrust of others. Individuals often interpret benign actions as malicious. This suspicion can lead to significant interpersonal difficulties.
Schizoid personality disorder presents with emotional detachment and limited social engagement. People with this condition may appear indifferent to praise or criticism, focusing instead on solitary activities.
In contrast, schizotypal personality disorder features eccentric behaviors and cognitive distortions. These individuals may exhibit odd beliefs or magical thinking while struggling with intense discomfort in close relationships.
Careful assessment using structured interviews and standardized questionnaires helps clarify these distinctions. Mental health professionals must consider the patient’s history and behavior patterns for accurate diagnosis.
Evidence-Based Treatment Approaches for Cluster A Personality Disorders
Treating Cluster A Personality Disorders requires a nuanced approach. Evidence-based therapies focus on improving emotional regulation and interpersonal skills.
Cognitive Behavioral Therapy (CBT) is often effective. It helps individuals identify distorted thinking patterns and develop healthier coping mechanisms. This method can lead to better social interactions.
Another promising approach is Dialectical Behavior Therapy (DBT). Originally designed for borderline personality disorder, DBT teaches mindfulness and distress tolerance, which can be beneficial for those with cluster A traits as well.
Medications may also play a role. Antipsychotics or antidepressants are sometimes prescribed to manage symptoms like anxiety or mood fluctuations. These should always accompany therapy for optimal results.
Group therapy offers a supportive environment where individuals can share experiences. Building connections with others facing similar challenges fosters understanding and reduces isolation, making treatment more impactful.
Challenges in Engaging Cluster A Individuals in Treatment
Engaging individuals with Cluster A Personality Disorders in treatment poses significant challenges. Their inherent distrust and suspicious nature often make them resistant to therapy. This skepticism can lead to avoidance of mental health services altogether.
Additionally, people with these disorders may struggle to recognize that they have a problem requiring intervention. They might perceive their thoughts and behaviors as normal, which complicates the process of seeking help.
Building rapport is crucial yet difficult. Therapists must navigate issues of paranoia or emotional detachment while fostering a safe environment for open dialogue.
Moreover, the eccentricities associated with these disorders can manifest in unpredictable behavior during sessions, making consistent engagement more complex. Tailored approaches are necessary to address their unique needs effectively while ensuring they feel understood and respected throughout the therapeutic journey.
Prognosis and Long-Term Outcomes for Cluster A Disorders
The prognosis for individuals with Cluster A personality disorders can vary widely. Some may experience significant challenges throughout their lives, while others might find ways to manage their symptoms effectively.
Long-term outcomes often depend on several factors. Early intervention and therapy can lead to better adaptation skills. Individuals who engage in consistent treatment are more likely to experience improvements in functioning and social interactions.
However, many face ongoing difficulties due to the nature of these disorders. Social withdrawal or peculiar behaviors can hinder relationships and career advancement.
Support systems play a crucial role in recovery; those with strong networks tend to fare better over time. It’s essential for caregivers and loved ones to understand these dynamics, fostering an environment conducive to healing and growth without judgment or stigma.
Cultural Variations in the Expression of Cluster A Traits
Cultural context significantly influences how Cluster A personality disorders manifest. Different societies have varying norms surrounding social behavior, which can affect perceptions of odd or eccentric traits.
For instance, in some cultures, behaviors considered schizotypal—such as magical thinking or unconventional beliefs—may be viewed as spiritual rather than pathological. This cultural lens can lead to different interpretations and responses to these traits.
Moreover, collectivist societies might emphasize conformity and group harmony more than individualistic ones. Therefore, those exhibiting paranoid tendencies may experience heightened stigma in environments where trust is crucial for community cohesion.
Understanding these cultural dimensions helps clinicians appreciate the nuances of diagnosis and treatment. It also fosters a more empathetic approach when interacting with individuals displaying Cluster A characteristics across diverse backgrounds.
Comorbidities: Cluster A Disorders and Other Mental Health Conditions
Individuals with Cluster A personality disorders often exhibit comorbidities with other mental health conditions. This overlap can complicate diagnosis and treatment.
For instance, many people diagnosed with paranoid personality disorder may also experience anxiety disorders. The constant state of suspicion can heighten feelings of fear or apprehension.
Schizoid personality disorder frequently coexists with depressive disorders. Those showing little interest in social relationships might struggle internally, leading to pervasive sadness.
Schizotypal personality disorder is particularly associated with psychotic experiences and is sometimes found alongside schizophrenia spectrum disorders. These individuals may face challenges that blur the lines between their unique thoughts and more severe psychotic symptoms.
Recognizing these comorbidities is vital for effective intervention strategies tailored to individual needs. Treatment plans must address both the primary cluster A disorder and any accompanying mental health issues to improve overall outcomes.
Future Research Directions in Cluster A Personality Disorders
As we look toward the future of research in Cluster A Personality Disorders, several promising avenues emerge. First, there is a pressing need for longitudinal studies that track individuals over time to better understand the development and progression of these disorders. This approach can provide insights into how symptoms evolve and inform treatment approaches.
Additionally, interdisciplinary collaboration between psychologists, neuroscientists, and geneticists could yield breakthroughs in understanding the biological underpinnings of these disorders. Exploring neuroimaging techniques may help identify specific brain structures or functions associated with Cluster A traits.
Moreover, investigations into cultural contexts are essential. Understanding how different cultures perceive odd or eccentric behaviors can enhance diagnostic accuracy and improve therapeutic relationships across diverse populations.
More randomized controlled trials focusing on tailored interventions will be critical. These should aim to address both symptom management and enhancement of social functioning for those affected by these personality disorders.
Research in this area holds great potential not only for improving clinical practices but also for fostering greater awareness about the experiences of individuals living with Cluster A Personality Disorders.