Understanding the complexities of human behavior can often feel like navigating a labyrinth. Among the many psychological conditions that pique interest, Antisocial Personality Disorder (ASPD), psychopathy, and sociopathy stand out due to their overlapping traits yet distinct characteristics. These terms are frequently used interchangeably in popular culture, but doing so overlooks important nuances.
Have you ever wondered how they truly differ? What sets ASPD apart from psychopathy and sociopathy? By delving into these disorders’ definitions, symptoms, and underlying factors, we can unravel this intricate web of personality disorders. Join us as we explore what makes each condition unique while shedding light on their similarities and societal implications.
Defining Antisocial Personality Disorder (ASPD)
Antisocial Personality Disorder (ASPD) is characterized by a pervasive pattern of disregard for the rights of others. Individuals with ASPD often show impulsive behaviors, lack empathy, and exhibit deceitful tendencies.
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines specific criteria for diagnosing this disorder. Symptoms typically include aggressive behavior, rule-breaking actions, and a tendency to manipulate or exploit others without remorse.
Research suggests that ASPD affects about 1% of the general population, though prevalence may be higher among certain demographic groups. It’s more commonly diagnosed in men than women.
Key behavioral patterns include irritability, aggression, and irresponsibility in work or financial matters. Those with ASPD may struggle to maintain long-term relationships due to their self-centered nature. Understanding these traits contributes significantly to recognizing how they impact interpersonal dynamics and societal interactions.
Diagnostic criteria in DSM-5
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), outlines specific criteria for diagnosing Antisocial Personality Disorder (ASPD). To qualify, a person must exhibit a pervasive pattern of disregard for the rights of others. This behavior typically begins in childhood or early adolescence.
Individuals with ASPD often engage in deceitfulness, impulsivity, irritability, and aggressiveness. They may also demonstrate a lack of remorse for their actions. The DSM-5 emphasizes that these traits should significantly impair social functioning or lead to legal issues.
A key component is that these behaviors cannot solely be attributed to developmental disorders or substance use. Clinicians look at patterns over time to ensure an accurate diagnosis rather than focusing on isolated incidents. Hence, understanding these criteria helps mental health professionals identify individuals who may require intervention and support effectively.
Prevalence and demographic factors
Antisocial Personality Disorder (ASPD) affects a significant segment of the population. Research indicates that around 1% to 4% of adults suffer from this disorder, with higher prevalence rates in clinical settings.
Demographic factors play a crucial role in understanding ASPD. It tends to be more prevalent in males than females, often with ratios ranging from 3:1 to as high as 6:1. This disparity may relate to societal norms surrounding aggression and emotional expression.
Age is another important factor; symptoms typically emerge during late adolescence or early adulthood. However, some individuals may show signs earlier in life, particularly during childhood conduct disorders.
Cultural context also influences how ASPD presents and is diagnosed. Different societies have varying thresholds for acceptable behavior, impacting recognition and reporting of symptoms across diverse populations.
Key behavioral patterns and symptoms
Individuals with Antisocial Personality Disorder (ASPD) often exhibit a range of troubling behaviors. One notable pattern is persistent disregard for societal norms and rules. This can manifest as illegal activities, deceitful behavior, or manipulation.
Impulsivity is another key symptom. Those affected may struggle to plan ahead or consider the consequences of their actions. This impulsiveness can lead to reckless decisions that endanger themselves and others.
Interpersonal relationships are frequently shallow or exploitative. A lack of empathy makes forming genuine connections difficult, leading to increased conflict and instability in personal interactions.
Additionally, irritability and aggressive tendencies are common. Frequent outbursts may result from perceived slights or frustrations, escalating into physical altercations at times.
These behavioral patterns contribute significantly to the challenges faced by individuals diagnosed with ASPD, affecting their quality of life and interactions within society.
Exploring Psychopathy
Psychopathy is often characterized by a distinct set of traits that set it apart from other personality disorders. Core characteristics include superficial charm, high intelligence, and an inherent lack of empathy. Individuals with psychopathic tendencies can manipulate others skillfully while displaying a shallow range of emotions.
The Hare Psychopathy Checklist-Revised (PCL-R) is the primary assessment tool used to evaluate these traits. This diagnostic instrument comprises multiple items focusing on interpersonal skills, affective responses, and lifestyle choices. Scoring helps determine the severity of psychopathic traits in individuals.
Understanding psychopathy also involves recognizing how societal perceptions shape its stigma. Often portrayed in media as violent or criminally inclined, this portrayal oversimplifies the condition and neglects subtler dimensions that can manifest in daily life or corporate settings. Thus, exploring psychopathy requires a nuanced approach beyond just labels or stereotypes.
Core traits and characteristics
Psychopathy is marked by a distinct set of core traits and characteristics. Individuals with psychopathic tendencies often exhibit superficial charm, allowing them to easily manipulate others. This façade can mask their underlying emotional deficits.
A lack of empathy is another hallmark trait. Psychopaths struggle to understand or relate to the feelings of others, which enables cold and calculated decision-making. They may act ruthlessly in pursuit of their goals.
Impulsivity also plays a significant role in psychopathy. These individuals may engage in risky behaviors without considering the consequences, demonstrating poor behavioral control.
Additionally, grandiosity is common among psychopaths. They tend to hold an inflated sense of self-worth and believe they are superior to those around them. Their need for stimulation drives them toward thrill-seeking activities that can escalate into dangerous situations.
Understanding these traits helps differentiate psychopathy from other personality disorders, particularly when assessing behavior patterns.
The PCL-R assessment tool
The Hare Psychopathy Checklist-Revised (PCL-R) is a clinical tool designed to measure psychopathic traits in individuals. Developed by Dr. Robert Hare, it consists of 20 items that evaluate affective and interpersonal characteristics.
Each item is scored on a scale from 0 to 2 based on the presence and severity of specific traits. The total score can range from 0 to 40, with higher scores indicating stronger psychopathic tendencies.
Key areas assessed include superficial charm, lack of remorse, manipulative behaviors, and emotional detachment. This comprehensive evaluation helps mental health professionals differentiate between psychopathy and other personality disorders.
Moreover, the PCL-R has been widely used in forensic settings to inform criminal profiling and risk assessments. Its insights are invaluable for understanding an individual’s propensity for violence or recidivism within legal contexts.
Unraveling Sociopathy
Sociopathy, often conflated with antisocial personality disorder (ASPD), has distinct origins and characteristics. It’s believed to arise from a combination of environmental factors, such as upbringing and traumatic experiences.
Unlike psychopathy, individuals labeled as sociopaths can form attachments to specific people or groups. Their emotional responses are generally more volatile and unpredictable compared to the calculated demeanor of psychopaths.
Behaviorally, sociopaths may act impulsively and exhibit signs of anger or aggression easily. This unpredictability makes it challenging for them to maintain stable relationships or employment.
Societal perceptions also differ; sociopaths are often viewed with a mix of fear and pity due to their visible struggles. These individuals may be seen as products of their environment rather than inherently malicious. Understanding these nuances helps in addressing misconceptions surrounding sociopathy within broader discussions on mental health.
Origins and conceptual development
Sociopathy has its roots in early psychological theories that sought to understand deviant behavior. The term emerged in the early 20th century, primarily associated with discussions around social and environmental influences on human conduct.
As research progressed, sociopathy was distinguished from other personality disorders by emphasizing the role of upbringing and trauma. This perspective suggested that individuals may develop sociopathic traits as a response to adverse experiences during formative years.
Unlike psychopathy, which is often linked to innate biological factors, sociopathy points more toward societal context. This shift reflected an evolving understanding of how personal history shapes behavioral patterns.
The conceptual development of sociopathy continues today. It grapples with complexities surrounding moral responsibility and the interplay between genetics and environment in shaping antisocial behaviors. As society becomes increasingly aware of these intricacies, definitions continue to adapt accordingly.
Distinguishing features and behaviors
Sociopathy exhibits distinct features that set it apart from related disorders. Individuals with sociopathy often demonstrate a blatant disregard for social norms and rules. This rebelliousness can manifest in impulsive behaviors and erratic emotional responses.
Unlike those with psychopathy, who may appear charming and manipulative, sociopaths are more prone to outbursts of anger or frustration. Their relationships are marked by instability due to their unpredictable nature.
Another key behavior is the capacity for attachment. Sociopaths can form genuine emotional bonds but struggle to maintain them over time. Their lack of empathy leads to difficulties in understanding others’ emotions, further complicating personal connections.
In many cases, societal influences play a significant role in shaping a sociopath’s behavior. Environmental factors such as upbringing or trauma contribute significantly to their actions and interactions with others.
Societal impact and perceptions
Societal impact and perceptions surrounding sociopathy are complex. Many view individuals with sociopathic traits as dangerous due to their disregard for societal norms. This stereotype can contribute to stigmatization, leading to misunderstandings about the disorder.
Media portrayals often amplify these fears, depicting sociopaths as cold-blooded criminals or manipulators. Such representations can skew public perception, overshadowing the nuanced reality of those affected by this condition.
In workplaces and communities, people may feel cautious or wary around individuals displaying sociopathic behaviors. This apprehension can hinder social integration and create barriers to empathy and support for those struggling with their symptoms.
Education plays a pivotal role in reshaping these views. Increased awareness about mental health conditions fosters compassion rather than fear. Promoting understanding helps dismantle stereotypes associated with sociopathy, encouraging acceptance within society.
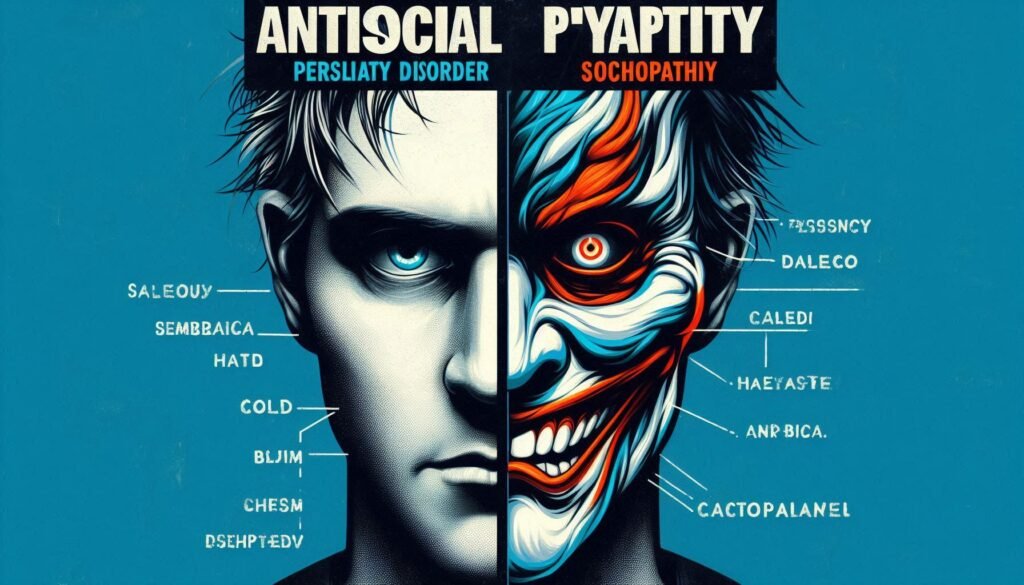
Comparative Analysis: ASPD, Psychopathy, and Sociopathy
Antisocial Personality Disorder (ASPD), psychopathy, and sociopathy share overlapping symptoms but are distinct in their manifestations. Individuals with ASPD often exhibit a pervasive pattern of disregard for others’ rights, while psychopaths display superficial charm and a lack of empathy.
Psychopaths tend to be more organized in their deceitful behaviors. They may plan their actions meticulously, showcasing higher levels of emotional detachment. In contrast, sociopaths can be impulsive and prone to outbursts due to emotional dysregulation.
Neurobiologically, differences arise as well. Research suggests that psychopathic traits are associated with specific brain abnormalities affecting emotion regulation and impulse control. Sociopaths might show heightened reactivity in areas linked to emotional responses.
Understanding these nuances aids clinicians in tailoring effective interventions for each condition’s unique challenges.
Overlapping symptoms and behaviors
Antisocial Personality Disorder (ASPD), psychopathy, and sociopathy share several overlapping symptoms. Individuals with these conditions often exhibit a disregard for societal norms and the rights of others. This can manifest as manipulative behavior or deceitfulness.
Impulsivity is another common trait. People affected may engage in risky activities without considering the consequences. Emotional detachment also plays a significant role; individuals may struggle to form genuine emotional connections with others.
Aggression is frequently observed across all three disorders. It can be expressed through verbal outbursts or physical violence, depending on the individual’s circumstances and environment.
Additionally, lack of remorse for harmful actions links these disorders together. Many individuals do not experience guilt when they cause harm or distress to others, which complicates their relationships and social interactions further.
Key differentiating factors
When exploring how Antisocial Personality Disorder (ASPD) differs from psychopathy and sociopathy, it’s essential to identify key differentiating factors.
Individuals with ASPD often exhibit a broader range of behaviors that violate societal norms, including deceitfulness and impulsivity. These traits manifest in various antisocial acts throughout their lives.
Psychopaths typically display more calculated behavior. They are often charming and can manipulate others effectively. Their emotional detachment allows them to engage in harmful actions without remorse or anxiety about consequences.
Sociopaths, on the other hand, may form attachments but struggle to maintain relationships due to erratic behavior and frequent outbursts of anger. This emotional volatility sets them apart from both ASPD individuals and psychopaths.
Understanding these nuances aids not only in accurate diagnosis but also informs tailored treatment approaches for each condition.
Neurocognitive and neurobiological distinctions
Neurocognitive and neurobiological distinctions play a crucial role in understanding how Antisocial Personality Disorder (ASPD), psychopathy, and sociopathy differ. Research indicates that individuals with ASPD often show deficits in emotional processing and empathy. This can be linked to abnormalities in brain regions such as the amygdala, which is essential for emotion regulation.
On the other hand, psychopathy is associated with more significant impairments in moral reasoning and affective responses. Neuroimaging studies reveal reduced activation in areas like the prefrontal cortex among psychopaths, leading to impulsivity and lack of remorse.
Sociopaths tend to exhibit heightened emotional sensitivity compared to their counterparts. Their neurobiological makeup may reflect increased stress reactivity, making them prone to erratic behaviors influenced by environmental factors rather than innate neurological deficits.
These differences highlight why accurate diagnosis requires nuanced understanding beyond surface-level behavioral traits. Each condition presents unique challenges related to treatment and management strategies.
Diagnostic Challenges and Controversies
Diagnosing Antisocial Personality Disorder (ASPD) presents numerous challenges. The overlapping symptoms with psychopathy and sociopathy can complicate clinical assessments. Mental health professionals often face difficulty in distinguishing these conditions, leading to potential misdiagnosis.
There is ongoing debate within psychiatric communities about the validity of ASPD as a distinct diagnosis. Some argue that it should encompass psychopathic traits or even be merged with sociopathy due to their shared characteristics.
Cultural perceptions also influence diagnostic criteria. Different societies may interpret behaviors differently, impacting how individuals are assessed and diagnosed globally.
Furthermore, stigma plays a significant role in treatment approaches for those diagnosed with ASPD, psychopathy, or sociopathy. This stigma could deter individuals from seeking help or lead clinicians to adopt biased views during assessment processes.
Issues in clinical assessment and diagnosis
Clinical assessment of Antisocial Personality Disorder (ASPD), psychopathy, and sociopathy presents several challenges. One prominent issue is the overlap in symptoms among these disorders. This can lead to misdiagnosis or confusion during evaluations.
Moreover, many individuals with these conditions may not seek help voluntarily. They often exhibit a lack of insight into their behaviors, making accurate self-reporting difficult. Clinicians must rely on third-party reports or historical data for a clearer picture.
Additionally, there are no definitive laboratory tests available to confirm diagnoses. Instead, professionals depend heavily on structured interviews and psychological assessments. The reliance on subjective judgment can introduce variability in outcomes.
Cultural factors also play a role in diagnosis complexity. Different backgrounds might influence how symptoms manifest or are perceived by clinicians, leading to potential biases in diagnostic practices.
Debates in psychiatric and psychological communities
Debates within psychiatric and psychological communities often arise around the definitions and distinctions between antisocial personality disorder (ASPD), psychopathy, and sociopathy. Experts frequently clash over whether these terms should be treated as distinct entities or variations of a single diagnosis.
Some professionals argue that labeling differences is essential for effective treatment strategies. They emphasize that understanding nuances can lead to better therapeutic outcomes. Others contend that such distinctions may complicate clinical practice without significant benefits in patient care.
Moreover, there are ongoing discussions about the role of genetics versus environmental factors in these disorders. Some researchers lean toward a biological basis affecting behavior, while others highlight socio-economic influences as pivotal contributors.
These debates create an evolving landscape where theories and practices continuously adapt to new findings, ensuring a dynamic approach to mental health diagnoses and treatments.
Implications for treatment approaches
Treatment approaches for individuals with Antisocial Personality Disorder (ASPD) can be quite complex. Traditional therapies often struggle to produce significant changes due to the lack of empathy and remorse associated with the condition.
Behavioral interventions focusing on social skills and impulse control might yield some positive outcomes. These therapies help individuals recognize harmful patterns in their behavior, fostering healthier interactions.
For psychopathy, treatment is even more challenging. Many professionals are skeptical about its effectiveness since psychopaths may manipulate therapeutic settings for personal gain rather than genuine change.
Sociopathy, meanwhile, may respond better to structured environments like rehabilitation programs. Consistent support and monitoring can assist sociopaths in developing better coping mechanisms.
These varying conditions necessitate tailored strategies that address specific traits and behaviors while considering individual differences among patients. Recognizing these nuances is crucial for effective intervention planning.
Treatment Approaches and Prognosis
Treatment for Antisocial Personality Disorder (ASPD) often involves a combination of psychotherapy and medication. Cognitive-behavioral therapy is commonly used to help individuals recognize harmful thoughts and behaviors. This approach encourages healthier coping mechanisms.
For psychopathy, treatment options are limited. Many professionals focus on managing symptoms rather than seeking a cure. Some therapies aim to improve emotional understanding and reduce manipulative behavior.
Sociopathy can also benefit from therapeutic interventions that emphasize relational skills. Group therapy might be particularly useful in fostering social connections.
Prognosis varies widely across the spectrum of these disorders. While some individuals may show improvement over time, others may continue to exhibit disruptive behaviors into adulthood. Early intervention tends to yield better outcomes, highlighting the importance of addressing these issues promptly during formative years.
Therapeutic interventions for ASPD
Therapeutic interventions for Antisocial Personality Disorder (ASPD) often focus on behavioral modification and cognitive restructuring. Cognitive Behavioral Therapy (CBT) is a primary approach, helping individuals recognize harmful thought patterns and develop healthier coping strategies.
Dialectical Behavior Therapy (DBT) can also be beneficial. It emphasizes emotional regulation and interpersonal effectiveness, aiding clients in managing distressing emotions more effectively.
Motivational interviewing plays a crucial role too. This client-centered technique encourages self-reflection, fostering motivation to change maladaptive behaviors.
Group therapy may provide additional support by creating an environment where individuals can learn from each other’s experiences. Engaging with peers offers opportunities for practicing social skills and receiving feedback in real time.
While these approaches show promise, success varies widely among individuals with ASPD due to the complexity of the disorder and its underlying traits.
Management strategies for psychopathy and sociopathy
Management strategies for psychopathy and sociopathy require a nuanced understanding of each disorder’s unique characteristics. Treatment approaches often emphasize behavioral management, as traditional therapy methods may yield limited success.
For individuals with psychopathy, the focus often lies in containment and supervision. Interventions might include structured environments that minimize opportunities for manipulative behaviors. Cognitive-behavioral techniques can help address specific maladaptive patterns, but progress is usually slow.
Sociopathic individuals may benefit more from social skills training and community-based interventions. These programs aim to enhance interpersonal relationships while promoting prosocial behaviors. Engaging them in group therapy can also facilitate insight into their actions and foster empathy through shared experiences.
Education plays a critical role across all treatment plans. Raising awareness among families, friends, and support networks about these disorders fosters an environment conducive to recovery or at least better management of symptoms.
The journey toward effective management is complex due to varying degrees of severity within each condition. Tailored strategies that consider individual needs are essential for improving outcomes in those living with antisocial personality traits.