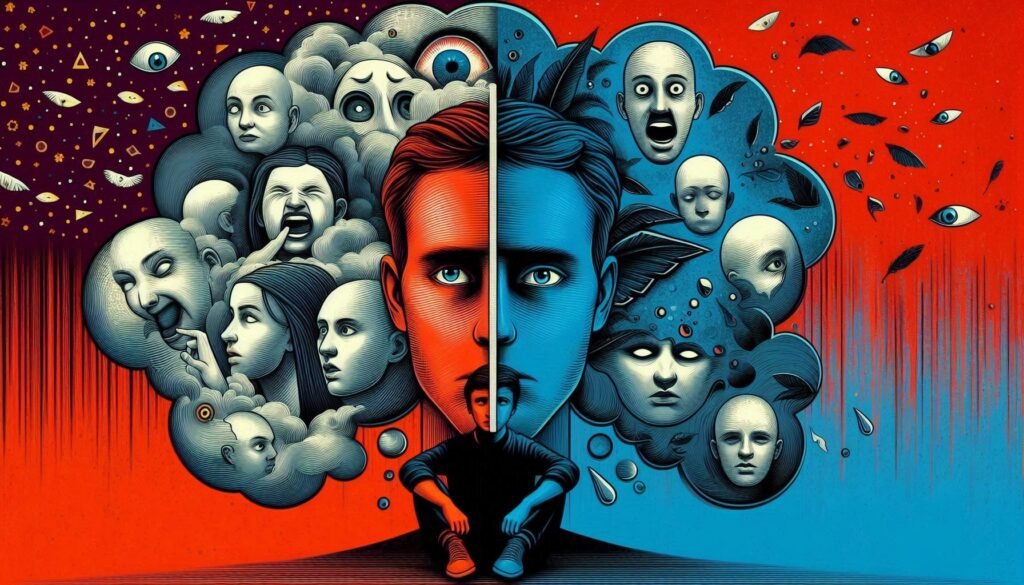
Paranoid Personality Disorder is a complex and often misunderstood mental health condition. It casts a long shadow over interpersonal relationships, creating obstacles that can feel insurmountable for those affected. Imagine navigating life with an ever-present sense of mistrust, where the intentions of others are seen through a lens of suspicion. This disorder not only impacts individuals but also reverberates through their families and communities.
As we delve into this topic, we’ll explore the key features that define Paranoid Personality Disorder and uncover its prevalence in society. We’ll also examine how genetics, environment, and neurobiology intertwine to shape these patterns of thought and behavior. Understanding this disorder requires looking beyond surface-level symptoms; it means recognizing the unique cognitive processes at play.
The journey will take us through various aspects such as diagnosis, treatment options, cultural considerations, and even long-term prognosis. By shedding light on Paranoid Personality Disorder today, we aim to foster greater awareness and empathy for those facing its challenges while providing valuable insights for better management strategies. Join us as we unravel the web of mistrust surrounding this intricate condition.

Defining Paranoid Personality Disorder: Key Features and Diagnostic Criteria
Paranoid Personality Disorder (PPD) is characterized by a pervasive pattern of distrust and suspicion towards others. Individuals with PPD often believe that others are out to harm or deceive them, even without clear evidence.
Key features include an unwavering belief that others’ motives are malevolent. They may interpret benign remarks as hostile and perceive personal slights in everyday interactions.
Diagnostic criteria outlined in the DSM-5 require these symptoms to be enduring, typically beginning in early adulthood. Affected individuals frequently exhibit hypervigilance, questioning loyalties and doubting the trustworthiness of friends and family members.
Additionally, they may struggle with emotional intimacy due to their fears of betrayal. This combination creates significant challenges in forming healthy relationships, leading to isolation and frustration over time. Understanding these core characteristics is essential for accurately identifying PPD and facilitating appropriate interventions.
The Epidemiology of Paranoid Personality Disorder: Prevalence and Risk Factors
Paranoid Personality Disorder (PPD) is more prevalent than many realize. Research suggests that it affects approximately 1% to 4% of the general population. This prevalence rate highlights how PPD remains an often-overlooked mental health issue.
Several risk factors contribute to its development. A family history of personality disorders can increase susceptibility, as genetics play a crucial role in shaping personality traits and behaviors.
Environmental influences are equally significant. Childhood trauma, neglect, or exposure to dysfunctional family dynamics can create fertile ground for paranoid ideation later in life.
Additionally, cultural context cannot be ignored; certain cultures may exhibit higher rates due to social and economic stressors that exacerbate feelings of mistrust and suspicion among individuals.
Understanding these epidemiological aspects is essential for effective intervention strategies and raising awareness about Paranoid Personality Disorder within communities.
Genetic and Environmental Contributions to Paranoid Personality Disorder
Genetic factors play a significant role in the development of Paranoid Personality Disorder. Research suggests that individuals with a family history of personality disorders may be at higher risk for developing paranoid traits. Genetic predispositions can influence neurotransmitter systems, which are critical in regulating mood and perception.
Environmental influences also contribute to this disorder’s emergence. Experiences during childhood, such as trauma or neglect, can shape one’s worldview. People exposed to chronic stress or unstable environments often develop heightened mistrust and suspicion toward others.
Additionally, cultural context cannot be overlooked. Societal norms and values can affect how paranoia is expressed and perceived. In some cultures, normative distrust might blur the lines between healthy skepticism and pathological paranoia.
The interplay between genetics and environment highlights the complexity of Paranoid Personality Disorder, making it essential to consider both aspects when examining its origins.
Neurobiological Underpinnings of Paranoid Ideation and Behavior
Neurobiological factors play a crucial role in understanding paranoid ideation and behavior. Research indicates that abnormalities in brain structures, particularly the amygdala and prefrontal cortex, may contribute to heightened mistrust.
The amygdala is involved in processing emotions and threat detection. In individuals with Paranoid Personality Disorder (PPD), this area can become hyperactive, leading to an exaggerated perception of danger from social interactions.
Additionally, the prefrontal cortex regulates decision-making and impulse control. Dysfunction here may impair one’s ability to assess situations accurately, fostering misinterpretations of others’ intentions.
Neurotransmitter systems are also essential players. Dysregulation of dopamine pathways has been linked to paranoia, suggesting that imbalances could exacerbate symptoms associated with PPD.
These neurobiological underpinnings highlight the complex interplay between brain function and paranoid thought processes, illustrating why effective treatment often requires a multifaceted approach.
Cognitive Patterns and Information Processing in Paranoid Personality Disorder
Individuals with Paranoid Personality Disorder often exhibit distinct cognitive patterns that shape their perceptions of the world. These individuals frequently interpret neutral or ambiguous situations as threatening. This hyper-vigilance can lead them to misread social cues, resulting in heightened suspicion.
Their information processing is marked by cognitive distortions. Such distortions may include jumping to conclusions and overgeneralizing experiences based on limited evidence. For instance, a brief encounter might be interpreted as betrayal rather than a simple misunderstanding.
Moreover, these thought processes reinforce a cycle of mistrust. As they perceive hostility where it does not exist, they often withdraw from others, further isolating themselves. This reinforces their beliefs and perpetuates feelings of paranoia.
Understanding these cognitive dynamics is crucial for effective treatment approaches aimed at breaking this cycle of mistrust and improving interpersonal functioning.
The Impact of Paranoid Personality Disorder on Interpersonal Relationships
Paranoid Personality Disorder significantly affects interpersonal relationships. Individuals with this condition often struggle to trust others, viewing their intentions as suspicious or hostile.
This pervasive distrust can lead to conflicts and misunderstandings. Friends and family may feel alienated due to the constant scrutiny of their actions. Open communication becomes difficult when every word is dissected for hidden meanings.
Romantic partnerships are particularly challenging. The fear of betrayal can create a barrier that prevents intimacy. Partners may feel they are walking on eggshells, unsure how to reassure someone whose trust is hard-earned.
Social situations often exacerbate these issues. People with Paranoid Personality Disorder might isolate themselves, fearing judgment or ridicule from peers. This withdrawal further deepens feelings of loneliness and frustration.
The ripple effects touch all aspects of life, making it crucial for individuals affected by this disorder to seek support in fostering healthier connections with others.
Differential Diagnosis: Distinguishing Paranoid PD from Other Disorders
Differentiating Paranoid Personality Disorder (PPD) from other mental health disorders can be challenging. Several conditions share overlapping symptoms, which complicates the diagnostic process.
For instance, schizophrenia may present with paranoid delusions, but this disorder involves more severe cognitive disruptions and hallucinations. PPD lacks these pronounced distortions of reality.
Similarly, anxiety disorders might feature heightened vigilance and mistrust. However, individuals with anxiety typically do not exhibit the pervasive suspicion characteristic of PPD.
Borderline personality disorder also warrants careful consideration due to impulsivity and turbulent relationships. Yet those with borderline traits often have fluctuating self-image and emotions that are less rigid than in PPD.
To accurately diagnose PPD, mental health professionals rely on comprehensive assessments that distinguish these nuanced differences. Detailed patient history and symptom evaluation are key components in making an accurate diagnosis.
Assessment Tools and Techniques for Diagnosing Paranoid Personality Disorder
Accurately diagnosing Paranoid Personality Disorder requires a nuanced approach. Clinicians often use structured interviews to gather comprehensive patient histories. This method encourages open dialogue, allowing individuals to express their feelings and thoughts in depth.
Standardized assessment tools play a crucial role as well. The Millon Clinical Multiaxial Inventory (MCMI) is commonly used for personality disorders, including paranoid traits. It helps identify specific patterns that align with the disorder’s characteristics.
Self-report questionnaires, like the Beck Anxiety Inventory, can also provide insights into an individual’s thought processes and emotional states. These instruments help gauge levels of anxiety and mistrust that accompany paranoid ideation.
In addition to these tools, clinicians must consider cultural contexts and individual differences during assessments. Understanding the patient’s background aids in distinguishing paranoia stemming from environmental factors versus clinical symptoms of Paranoid Personality Disorder.
Evidence-Based Treatment Approaches: Psychotherapy for Paranoid PD
Psychotherapy is a vital component in treating Paranoid Personality Disorder. It focuses on improving the individual’s coping mechanisms and fostering healthier thought patterns.
Cognitive-behavioral therapy (CBT) has shown promise for patients with paranoid traits. This approach helps individuals identify distorted thinking and replace it with more rational beliefs. Through guided discussions, therapists encourage clients to explore their feelings of mistrust.
Another effective method is schema-focused therapy, which delves into long-standing cognitive frameworks that contribute to paranoia. By addressing these core schemas, patients can begin to reshape their perceptions of others.
Group therapy offers an additional layer of support by providing a safe environment for social interaction. Sharing experiences with peers can reduce feelings of isolation and foster trust-building skills.
Psychotherapy aims not just at alleviating symptoms but also enhancing overall emotional resilience and interpersonal functioning in those affected by Paranoid Personality Disorder.
Pharmacological Interventions: The Role of Medication in Managing Symptoms
Pharmacological interventions play a significant role in managing symptoms of Paranoid Personality Disorder. Although there is no specific medication approved for this condition, clinicians often prescribe medications to alleviate associated anxiety and mood disturbances.
Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), may help reduce depressive symptoms that accompany paranoia. Additionally, antipsychotic medications can be effective in addressing severe paranoid ideation or psychotic features when present.
However, the use of these medications requires careful monitoring. Side effects can vary widely and impact adherence to treatment plans. Collaborating closely with healthcare providers ensures that patients receive tailored care suited to their unique needs.
Medications are generally most effective when combined with psychotherapy. This comprehensive approach provides individuals with tools to manage their thoughts and behaviors more effectively while minimizing reliance on pharmacological solutions alone.
Challenges in Treating Paranoid Personality Disorder: Building Trust
Treating Paranoid Personality Disorder (PPD) presents significant challenges, primarily due to the inherent mistrust that individuals with this condition experience. Building a therapeutic alliance is often difficult since patients may perceive therapists as potential threats or adversaries.
This constant suspicion can lead to resistance in therapy. Patients might reject feedback, question the therapist’s motives, and even sabotage their treatment progress. Establishing trust requires patience and consistent reassurance from mental health professionals.
Therapists must adapt their approach by demonstrating empathy while maintaining clear boundaries. It’s crucial to create a safe environment where clients feel secure enough to express their fears without judgment.
Strategies such as active listening and validating feelings can help foster trust over time. However, it demands ongoing effort from both parties to navigate the complexities of PPD effectively.
The Relationship Between Paranoid PD and Other Psychiatric Conditions
Paranoid Personality Disorder often intersects with various psychiatric conditions, complicating diagnosis and treatment. Individuals may exhibit symptoms overlapping with disorders such as schizophrenia or delusional disorder.
Anxiety disorders frequently co-occur, amplifying feelings of mistrust and fear. This heightened anxiety can exacerbate paranoid thoughts, leading to a cycle that’s difficult to break.
Additionally, mood disorders like depression can be present alongside Paranoid PD. The persistent feelings of suspicion may contribute to isolation and emotional distress.
Substance use disorders are also notable in this context. Some individuals turn to drugs or alcohol as coping mechanisms for their paranoia, which further complicates their mental health landscape.
Understanding these relationships is crucial for effective treatment strategies tailored to individual needs and experiences. Each person’s journey varies significantly, demanding a nuanced approach from healthcare providers.
Cultural Considerations in Diagnosing and Treating Paranoid PD
Cultural factors play a significant role in the diagnosis and treatment of Paranoid Personality Disorder. Different cultural backgrounds can shape how symptoms manifest and are perceived by both individuals and clinicians.
For instance, behaviors that may seem paranoid in one culture might be viewed as protective or cautious in another. This disparity underscores the importance of culturally sensitive assessments to avoid misdiagnosis.
Language barriers can also affect communication, leading to misunderstandings about intentions or feelings. Clinicians must be aware of these nuances to ensure accurate evaluations.
Moreover, cultural stigma surrounding mental health can hinder individuals from seeking help. Understanding these dynamics is crucial for effective intervention strategies that resonate with diverse populations.
Incorporating cultural competence into therapeutic practices fosters trust, encouraging clients to engage openly in their treatment journey.
Long-Term Prognosis and Quality of Life with Paranoid Personality Disorder
The long-term prognosis for individuals with Paranoid Personality Disorder can vary greatly. Many may experience persistent mistrust and suspicion throughout their lives, impacting personal and professional relationships.
Quality of life often suffers due to social isolation. Individuals might struggle to maintain friendships or romantic partnerships, leading to feelings of loneliness. Their pervasive distrust can also hinder career advancement.
Therapeutic interventions play a crucial role in improving outcomes. Engaging in psychotherapy can help challenge distorted thoughts and enhance emotional regulation skills.
Family support is equally vital in fostering understanding and patience during difficult times.
While some may find ways to adapt, others could face enduring challenges that significantly affect daily functioning and overall well-being. Continued research into effective treatment strategies remains essential for enhancing the quality of life for those affected by this disorder.
Future Directions in Research and Treatment of Paranoid PD
The future of research and treatment for Paranoid Personality Disorder (PPD) holds significant promise as mental health professionals strive to better understand this complex condition. Ongoing studies are focused on refining diagnostic criteria, which could lead to more accurate identification of PPD in diverse populations.
Innovative approaches in psychotherapy are also being explored. Therapists are investigating how cognitive-behavioral techniques can be adapted specifically for individuals with paranoid ideation. Developing trust within therapeutic relationships remains a crucial focus, given the inherent mistrust associated with PPD.
Moreover, researchers aim to explore the genetic and neurobiological aspects further. Understanding these factors may illuminate potential interventions that target the root causes rather than just managing symptoms.
Another area gaining traction is the integration of cultural perspectives into diagnosis and treatment frameworks. Recognizing that expressions of paranoia can vary across different cultures will enhance clinicians’ sensitivity and effectiveness when working with diverse client groups.
There is an increasing need for community-based programs focusing on education about PPD both for those affected by it and their families. Improving public awareness could reduce stigma and promote acceptance while facilitating early intervention strategies.
As we move forward, a multidisciplinary approach combining psychology, psychiatry, neuroscience, and social support seems essential in improving outcomes for individuals living with Paranoid Personality Disorder.