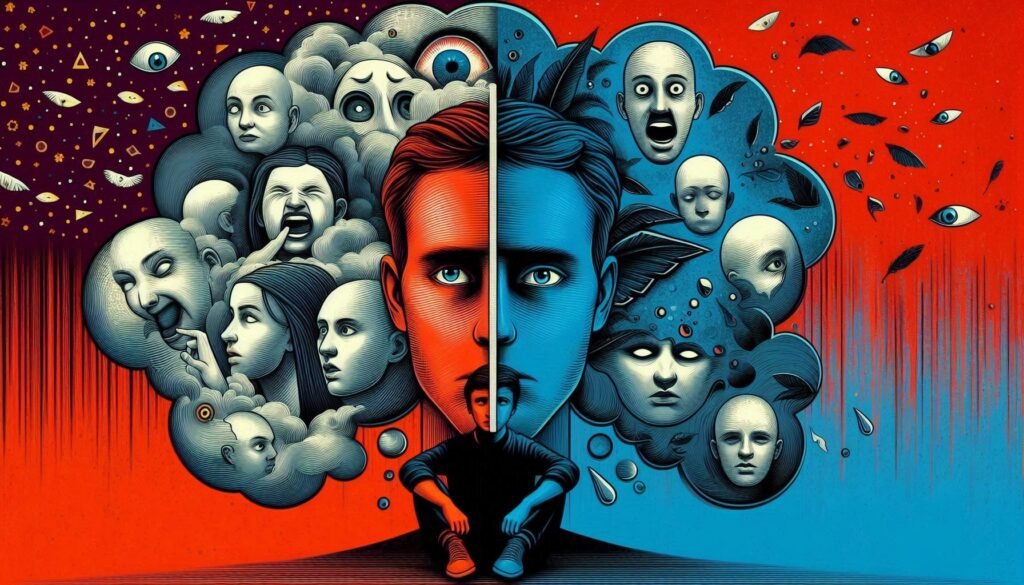
Understanding mental health can often feel like navigating a complex maze. Among the many disorders that exist, Paranoid Personality Disorder (PPD) and paranoid schizophrenia stand out due to their overlapping features and unique challenges. Both conditions can lead individuals to experience heightened suspicion or mistrust of others, but they stem from different origins and manifest in distinct ways.
This blog post delves into the differential diagnosis: PPD vs. paranoid schizophrenia, unraveling each disorder’s nuances. By exploring their symptoms, cognitive functioning, treatment options, and more, we aim to provide clarity for those affected by these conditions or seeking knowledge on mental health issues. Join us as we dissect these two complex disorders to better understand how they differ while recognizing the importance of accurate diagnosis in guiding effective treatment strategies.
Overview of Paranoid Personality Disorder (PPD)
Paranoid Personality Disorder (PPD) is characterized by a pervasive distrust and suspicion of others. Individuals with PPD often interpret benign remarks or actions as malevolent. This constant wariness can lead to strained relationships, both personal and professional.
People with PPD may believe that others are out to harm them or deceive them, even without evidence. Their rigid thinking patterns make it difficult for them to accept differing viewpoints or criticisms.
Emotional responses in those with PPD tend to be intense but hidden beneath the surface. They might appear aloof or detached while feeling deeply affected by perceived slights.
The onset typically occurs in early adulthood, affecting various aspects of life. While some individuals may function well in certain settings, their interpersonal difficulties often hinder overall quality of life. Understanding these traits is crucial for recognizing how they can impact an individual’s daily experiences.
Understanding Paranoid Schizophrenia
Paranoid schizophrenia is a subtype of schizophrenia that primarily involves intense paranoia and delusions. Individuals with this condition often experience hallucinations, typically auditory, leading them to hear voices that may threaten or belittle them.
These symptoms can significantly distort reality. The affected person may become highly suspicious of others, believing they are being persecuted or conspired against. This constant state of fear can lead to social withdrawal and isolation.
Unlike paranoid personality disorder (PPD), which is more about pervasive distrust in relationships without the presence of psychosis, paranoid schizophrenia includes more severe disruptions in thought processes. These disturbances can affect daily functioning.
Understanding these differences is crucial for effective treatment and support strategies tailored to each condition’s specific needs. Recognizing the signs early on aids in better management outcomes for those affected by paranoid schizophrenia.
Comparative Symptomatology
When examining the comparative symptomatology of Paranoid Personality Disorder (PPD) and paranoid schizophrenia, distinct differences emerge. PPD primarily involves pervasive distrust and suspicion towards others. Individuals may interpret benign remarks as malicious or feel perpetually on guard.
In contrast, paranoid schizophrenia manifests with more severe symptoms. Hallucinations and delusions often dominate this condition. While a person with PPD may harbor mistrust based solely on their perceptions, someone with paranoid schizophrenia might experience vivid auditory hallucinations reinforcing that distrust.
Another key difference lies in the intensity of beliefs held by individuals. In PPD, doubts about others stem from deep-seated personality traits rather than psychotic breaks experienced in schizophrenia. These deviations highlight how critical it is to distinguish between these two disorders when assessing mental health concerns effectively.
Reality Testing and Insight
Reality testing refers to an individual’s ability to distinguish between what is real and what is not. In the context of Paranoid Personality Disorder (PPD) and paranoid schizophrenia, this capacity varies significantly.
Individuals with PPD typically maintain a level of insight into their condition. They may understand that their suspicions are unfounded but still struggle with pervasive distrust. This awareness can lead them to rationalize or defend their beliefs while remaining skeptical about others’ intentions.
Conversely, those suffering from paranoid schizophrenia often experience impaired reality testing. Their delusions can feel entirely real, making it challenging for them to recognize the irrationality behind these thoughts. This lack of insight contributes to heightened distress and dysfunction in daily life.
The difference in reality testing has profound implications for treatment approaches and prognosis across both conditions, highlighting the importance of accurate diagnosis by mental health professionals.
Functional Impairment
Functional impairment varies significantly between individuals with Paranoid Personality Disorder (PPD) and those diagnosed with paranoid schizophrenia.
People with PPD often exhibit a heightened sense of suspicion, which can lead to difficulties in forming close relationships. This distrust may impact their job performance or social interactions but usually does not completely hinder daily functioning.
In contrast, individuals with paranoid schizophrenia experience more severe functional impairments. Their symptoms—such as delusions and hallucinations—can disrupt everyday activities like work or self-care. These disruptions are often profound enough to necessitate long-term support.
The degree of impairment is also influenced by the individual’s coping mechanisms and support systems. While some may manage well despite their condition, others struggle intensely, highlighting the need for tailored interventions based on specific needs.
Course of Illness
The course of illness for Paranoid Personality Disorder (PPD) typically involves a chronic pattern of distrust and suspicion. Individuals may experience persistent feelings that others are out to harm them, often leading to social isolation. This maladaptive behavior usually begins in early adulthood and can continue throughout life.
In contrast, paranoid schizophrenia presents a more episodic nature. Symptoms can emerge suddenly, often marked by acute psychotic episodes characterized by hallucinations or delusions. These episodes may vary in intensity and duration.
While PPD remains relatively stable over time, individuals with paranoid schizophrenia may find their symptoms fluctuate significantly. Treatment interventions play a crucial role in managing these conditions but differ markedly based on the diagnosis, affecting long-term outcomes and recovery trajectories.
Cognitive Functioning
Cognitive functioning varies significantly between individuals with Paranoid Personality Disorder (PPD) and those diagnosed with paranoid schizophrenia.
People with PPD often exhibit intact cognitive abilities, including reasoning and problem-solving skills. They may hold strong opinions but typically process information logically. However, their distorted perceptions can lead to misunderstandings in social interactions.
On the other hand, paranoid schizophrenia can be associated with cognitive deficits. These may manifest as difficulties in attention, memory recall, or executive functioning tasks. The presence of hallucinations or delusions can further impair an individual’s ability to think clearly.
These differences are crucial for diagnosis since they influence treatment options and rehabilitation strategies. Understanding how cognition plays a role helps tailor interventions effectively for each condition’s unique challenges and needs.
Social and Interpersonal Relationships
Social and interpersonal relationships are significantly affected in both Paranoid Personality Disorder (PPD) and paranoid schizophrenia, though the nature of these impacts varies.
Individuals with PPD often maintain a façade of social interaction while harboring deep distrust towards others. This skepticism can lead to strained relationships or isolation as they may misinterpret benign actions as hostile.
In contrast, those with paranoid schizophrenia may struggle more profoundly with interpersonal connections due to their psychotic symptoms. Hallucinations or delusions can cause them to perceive threats where none exist, making it challenging for them to engage meaningfully with family and friends.
Both conditions hinder effective communication. However, the level of insight into their condition also plays a pivotal role. Those with PPD might be aware of their mistrust but feel justified in it, while individuals suffering from paranoid schizophrenia might lack that awareness entirely.
Onset and Development
The onset and development of Paranoid Personality Disorder (PPD) typically manifests in early adulthood. Individuals often display pervasive distrust and suspicion towards others, which can intensify over time.
In contrast, paranoid schizophrenia usually emerges in late adolescence to early adulthood. The onset may be marked by a gradual decline in functioning or a sudden acute episode characterized by hallucinations or delusions.
Both disorders exhibit variability in their progression. PPD tends to remain stable throughout life, with some individuals learning coping strategies to manage their symptoms. In contrast, paranoid schizophrenia can fluctuate significantly; periods of exacerbation may alternate with phases of relative stability.
Understanding the timing and nature of symptom emergence is crucial for effective diagnosis and treatment planning for both conditions. Awareness of these developmental patterns helps mental health professionals tailor interventions appropriately.
Family History and Genetic Factors
Family history plays a crucial role in understanding both Paranoid Personality Disorder (PPD) and paranoid schizophrenia. Studies suggest that individuals with a family member diagnosed with one of these disorders may be at an increased risk for developing similar conditions.
Genetic factors are also significant in this context. Research indicates that hereditary traits can contribute to the likelihood of developing paranoid schizophrenia, highlighting potential genetic vulnerabilities. In contrast, PPD is less clearly linked to genetics but still suggests some familial patterns.
Additionally, environmental influences interact with genetic predispositions. Stressful life events or trauma within families can exacerbate symptoms for those genetically predisposed. Understanding these nuances helps clinicians assess risks more accurately while considering family dynamics during diagnostic evaluations.
Neurobiological Differences
Neurobiological differences play a significant role in distinguishing between Paranoid Personality Disorder (PPD) and paranoid schizophrenia. Research indicates that individuals with paranoid schizophrenia often exhibit distinct alterations in brain structure and function.
For instance, abnormalities in dopamine pathways are commonly observed in those diagnosed with paranoid schizophrenia. This neurotransmitter is crucial for regulating mood and perception, leading to the characteristic delusions experienced by these patients.
In contrast, people suffering from PPD may not show the same level of neurochemical imbalances. Their symptoms arise more from cognitive distortions rather than overt psychotic features.
Brain imaging studies have revealed variations as well; structural differences such as enlarged ventricles or reduced grey matter density are frequently noted in patients with schizophrenia but less so in those with PPD.
These neurobiological markers underline the importance of precise diagnostic practices when differentiating between these two disorders.
Treatment Approaches: Similarities and Differences
Treatment approaches for Paranoid Personality Disorder (PPD) and paranoid schizophrenia share some commonalities but also exhibit significant differences due to the nature of each condition.
Both disorders can benefit from psychotherapy. Cognitive Behavioral Therapy (CBT) is often employed, helping individuals challenge distorted thinking patterns. In PPD, therapy focuses on improving self-awareness and interpersonal skills.
Medication plays a crucial role in treating paranoid schizophrenia. Antipsychotics are typically prescribed to manage symptoms like delusions or hallucinations. For PPD, medication isn’t usually the first line of treatment; however, antidepressants may be considered if secondary issues arise.
Group therapy can be useful for both conditions but must be approached with care in cases of PPD due to potential mistrust towards others. The therapeutic alliance is vital for effective treatment success across both disorders.
Prognosis and Long-term Outcomes
The prognosis for individuals with Paranoid Personality Disorder (PPD) varies significantly from that of those diagnosed with paranoid schizophrenia. PPD often allows for better long-term functioning, as individuals may maintain their insight and self-awareness about their condition.
In contrast, paranoid schizophrenia can lead to more severe impairments in daily life. Symptoms such as delusions and hallucinations can disrupt work and personal relationships. The course of this disorder is often chronic, with potential relapses despite treatment.
For both conditions, early intervention plays a crucial role in improving outcomes. Access to therapy and medication can help manage symptoms effectively.
However, the social stigma surrounding these disorders remains a significant barrier. Those affected may face challenges beyond just clinical symptoms—issues like isolation or difficulty maintaining relationships are common across both diagnoses. Long-term support networks are vital for enhancing quality of life for individuals battling either disorder.
Assessment Techniques and Diagnostic Tools
Accurate assessment techniques and diagnostic tools are vital for distinguishing between Paranoid Personality Disorder (PPD) and paranoid schizophrenia. Clinicians often start with comprehensive clinical interviews, where they gather detailed histories of symptoms and behaviors.
Standardized questionnaires can also be beneficial. Tools like the Millon Clinical Multiaxial Inventory (MCMI) help in assessing personality disorders, while instruments such as the Positive and Negative Syndrome Scale (PANSS) evaluate psychotic symptoms related to schizophrenia.
Observation plays a crucial role too. A clinician might note how patients interact during sessions, revealing insights into their thought processes and social functioning.
Additionally, neuropsychological testing may provide further clarity on cognitive impairments that could support a diagnosis. Combining multiple assessment strategies ensures a more accurate differential diagnosis between PPD and paranoid schizophrenia. This thorough approach is essential for effective treatment planning tailored to individual needs.
Importance of Accurate Differential Diagnosis
Accurate differential diagnosis between Paranoid Personality Disorder (PPD) and paranoid schizophrenia is crucial for effective treatment. Misdiagnosis can lead to inappropriate interventions that may exacerbate symptoms or neglect the underlying conditions.
Both disorders share some overlapping features, such as distrust and suspicion of others. However, they differ significantly in their severity and impact on functioning. PPD typically presents with enduring patterns of behavior rooted in personality traits, while paranoid schizophrenia involves more acute psychotic episodes characterized by delusions and hallucinations.
Effective assessment techniques are vital. Clinicians must utilize structured interviews, psychological evaluations, and observational data to tease apart these nuanced differences. Understanding a patient’s history—along with familial patterns—can provide insights into their condition.
Furthermore, accurate diagnosis informs treatment plans tailored specifically to each disorder’s unique challenges. For PPD, psychotherapy aimed at improving interpersonal skills might be beneficial. In contrast, patients diagnosed with paranoid schizophrenia often require a combination of medication management alongside therapeutic support.
The implications extend beyond individual care; proper classification enhances research efforts focused on etiology and therapeutic strategies for both disorders. Ensuring an accurate differential diagnosis not only improves patient outcomes but also contributes to broader societal awareness regarding mental health complexities.



