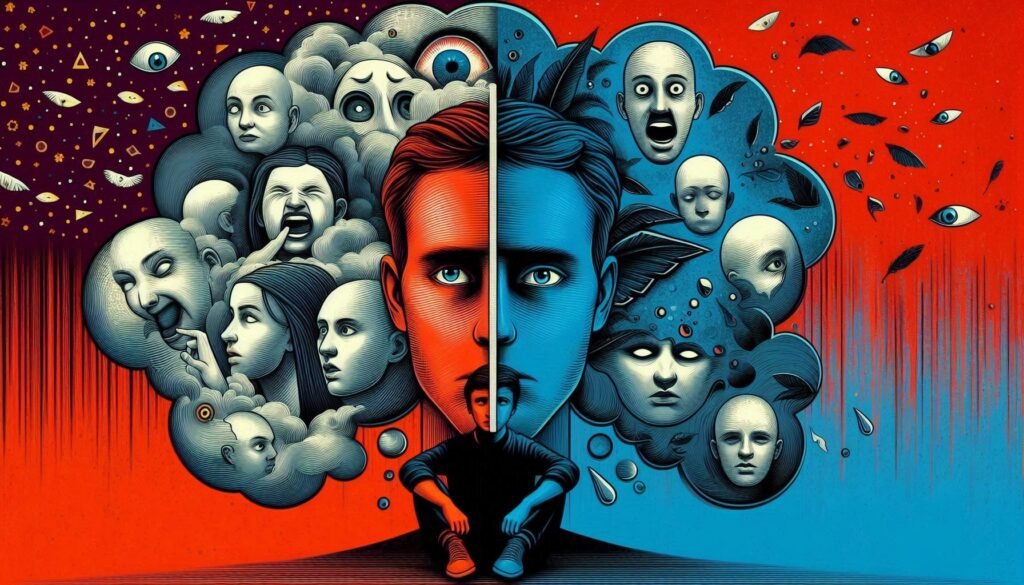
Schizoid Personality Disorder is often misunderstood, shrouded in ambiguity and stigma. Individuals with this disorder tend to navigate life differently, preferring solitude over social engagement. While some may view their withdrawn nature as aloofness or indifference, it’s crucial to recognize the depth of their experience and the complexities that lie beneath the surface.
In a world that increasingly values social connectivity, those with Schizoid Personality Disorder can be overlooked or mischaracterized. Understanding this condition opens up avenues for empathy and support. This blog post aims to demystify Schizoid Personality Disorder by exploring its core features, prevalence, genetic influences, emotional processing challenges, treatment options, and much more. Join us on this informative journey as we uncover what it truly means to live with Schizoid Personality Disorder while shedding light on a path toward greater awareness and acceptance.

Understanding Schizoid Personality Disorder: Definition and Core Features
Schizoid Personality Disorder is characterized by a pervasive pattern of detachment from social relationships and a restricted range of emotional expression. Individuals with this disorder often prefer solitary activities, finding comfort in their own company rather than seeking out social interactions.
Core features include limited interest in forming close relationships, which can lead to an apparent lack of desire for intimacy or romance. These individuals may appear indifferent to praise or criticism and usually have difficulty expressing emotions.
People with Schizoid Personality Disorder often display a rich inner world but struggle to connect it with others. Their detachment can sometimes be mistaken for aloofness, yet it stems from genuine discomfort in social situations rather than intentional disconnection. Understanding these defining traits helps foster empathy toward those navigating life through the lens of schizoids’ unique experiences.
The Prevalence and Demographics of Schizoid Personality Disorder
Schizoid Personality Disorder (SPD) is often overlooked in discussions of mental health. Its prevalence is estimated to be around 3-5% in the general population, making it relatively uncommon compared to other personality disorders.
Demographically, SPD tends to appear more frequently in males than females. This gender disparity raises questions about potential biological and social factors influencing its development.
Age-wise, symptoms typically manifest in early adulthood but may become more pronounced over time. Individuals with SPD often prefer solitude and display emotional detachment from others, leading to challenges in forming relationships.
Cultural context also plays a significant role. Variations exist based on societal norms regarding social behavior and emotional expression. Understanding these demographic nuances can provide insight into the lived experiences of those affected by Schizoid Personality Disorder.
Genetic and Environmental Factors in the Development of Schizoid PD
Genetic factors play a significant role in the development of Schizoid Personality Disorder. Research indicates that individuals with a family history of personality disorders may have an increased risk of developing schizoid traits.
Environmental influences also contribute to this complex condition. Childhood experiences, such as emotional neglect or trauma, might impact social engagement and interpersonal relationships later in life.
Attachment styles formed during early years can shape one’s ability to connect with others. A lack of nurturing environments often leads to withdrawal behaviors seen in those with schizoid characteristics.
Moreover, societal expectations can further exacerbate these tendencies. Cultural contexts that value independence over community connection may foster isolation among individuals predisposed to this disorder.
Understanding these genetic and environmental interactions is crucial for addressing Schizoid Personality Disorder effectively. It highlights the need for personalized approaches in both diagnosis and treatment.
Neurobiology of Schizoid Personality Disorder: Brain Structure and Function
Research into the neurobiology of Schizoid Personality Disorder reveals intriguing insights about brain structure and function. Neuroimaging studies suggest that individuals with this disorder may exhibit variations in specific brain regions associated with social cognition and emotional processing.
The prefrontal cortex, which governs decision-making and social behavior, often shows altered activity levels in those diagnosed with Schizoid PD. These differences can contribute to challenges in engaging socially or expressing emotions effectively.
Additionally, the limbic system plays a crucial role in emotion regulation. Abnormalities here might explain why individuals with Schizoid PD prefer solitary activities over interpersonal interactions.
Functional connectivity within these neural circuits also appears compromised, potentially leading to diminished empathetic responses. As our understanding deepens, exploring how these neurobiological factors intertwine will enhance therapeutic approaches for managing this complex condition.
Emotional Processing and Expression in Individuals with Schizoid PD
Individuals with Schizoid Personality Disorder often experience emotional processing in a distinct manner. Many report feeling detached from their emotions, which can result in difficulty recognizing or expressing feelings.
This emotional blunting may lead to challenges in relationships. Interactions are frequently perceived as burdensome rather than enjoyable. Consequently, these individuals tend to maintain distance from social situations.
Despite this detachment, some may possess an inner world rich with thoughts and fantasies. They might engage deeply with their ideas but struggle to share these experiences with others.
Understanding their unique perspective on emotions is vital for effective support. Therapeutic approaches must consider this nuanced relationship with feelings while fostering meaningful connections within safe environments. Encouraging expression through creative outlets can also prove beneficial in navigating complex emotions more comfortably.
Social Withdrawal and Interpersonal Dynamics in Schizoid Personality Disorder
Individuals with Schizoid Personality Disorder often experience significant social withdrawal. They tend to prefer solitude over engaging in social activities. This preference can be misinterpreted as shyness or aloofness.
Interpersonal dynamics for those with this disorder are complex. While they may desire minimal contact, their lack of emotional expression can create misunderstandings. Friends and family might feel rejected or confused by the person’s behavior.
In relationships, schizoids often remain detached. They find it challenging to establish deep connections, which can lead to feelings of isolation. Despite this, some individuals may form a few close bonds but still maintain a sense of distance.
This unique approach to relationships shapes their daily interactions. Understanding these dynamics is crucial for friends and loved ones who seek connection without overwhelming the individual experiencing symptoms of Schizoid Personality Disorder.
Diagnostic Criteria and Assessment Methods for Schizoid PD
Diagnosing Schizoid Personality Disorder (PD) requires a comprehensive evaluation by mental health professionals. The diagnostic criteria, as outlined in the DSM-5, include a pervasive pattern of detachment from social relationships and a restricted range of emotional expression.
Individuals often display preferences for solitary activities over interpersonal engagement. They may appear indifferent to praise or criticism and lack close friends outside immediate family members. This emotional flatness can make it challenging for clinicians to assess the disorder fully.
Assessment methods typically involve structured interviews and standardized questionnaires designed to gauge personality traits and functioning. Clinicians also gather historical information about an individual’s behavior patterns and relationships over time.
Understanding these criteria is essential for accurate diagnosis, as many symptoms overlap with other disorders such as avoidant personality disorder or autism spectrum conditions. A thorough assessment ensures that individuals receive appropriate care tailored to their specific needs.
Differential Diagnosis: Distinguishing Schizoid PD from Similar Conditions
Differentiating Schizoid Personality Disorder from similar conditions is crucial for accurate diagnosis and treatment. One commonly confused disorder is Avoidant Personality Disorder. Individuals with avoidant traits often desire social interaction but fear criticism, leading to withdrawal. In contrast, those with schizoid personality disorder typically show indifference toward relationships.
Another condition to consider is Autism Spectrum Disorder (ASD). While both may involve social difficulties, ASD usually includes challenges in communication and repetitive behaviors that are not characteristic of schizoid traits.
Additionally, Schizotypal Personality Disorder shares some similarities regarding eccentric behavior and social anxiety. However, individuals with schizotypal PD also experience perceptual distortions or odd beliefs which distinguish them from those diagnosed with a schizoid personality.
Proper assessment by mental health professionals helps clarify these distinctions through comprehensive interviews and standardized criteria. Understanding the nuances between these disorders enables tailored interventions that can significantly improve an individual’s quality of life.
Treatment Approaches: Psychotherapy Techniques for Schizoid Personality Disorder
Psychotherapy plays a crucial role in treating Schizoid Personality Disorder. Techniques like cognitive-behavioral therapy (CBT) help individuals identify and challenge distorted thoughts about relationships and social interactions.
Another effective approach is psychodynamic therapy, which delves into underlying emotions and unconscious processes. This method can foster self-awareness by exploring past experiences that shape current behaviors.
Group therapy may also benefit those with schizoid traits. It offers a safe space to practice interpersonal skills alongside others facing similar challenges. While group settings can be daunting, they promote gradual exposure to social situations.
Additionally, mindfulness-based therapies teach emotional regulation techniques. Learning to stay present can empower individuals to navigate their feelings without becoming overwhelmed.
Tailoring these approaches based on individual needs enhances effectiveness. A collaborative therapeutic relationship fosters trust, encouraging exploration of personal experiences at one’s own pace.
The Role of Medication in Managing Schizoid PD Symptoms
Medication can play a supportive role in managing symptoms associated with Schizoid Personality Disorder. While there is no specific medication approved for this condition, certain drugs may help alleviate co-occurring symptoms such as anxiety or depression.
Antidepressants like selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed to address mood-related issues. These medications can help improve emotional regulation and reduce feelings of hopelessness.
In some cases, antipsychotics might be used off-label. They can assist individuals who experience significant detachment or have difficulty engaging with reality.
It’s essential to tailor the approach based on individual needs. Regular consultations with mental health professionals ensure that any treatment plan remains effective and safe.
Though medication alone cannot resolve the core features of Schizoid PD, it offers relief from distressing symptoms, making daily life more manageable for those affected by this disorder.
Challenges in Engaging Schizoid Individuals in Treatment
Engaging individuals with Schizoid Personality Disorder in treatment poses unique challenges. Many prefer solitude and may view social interaction, including therapy sessions, as unnecessary or uncomfortable. This resistance can hinder their engagement in therapeutic processes.
Building a trusting relationship is crucial yet difficult. Those with schizoid traits often struggle to express emotions or share personal experiences. Therapists must navigate this barrier carefully.
Moreover, motivation for change can be limited. Individuals may not see their behavior as problematic. This ambivalence complicates the therapist’s role in fostering insight and encouraging participation.
Therapeutic approaches need to be tailored specifically for these clients. Traditional methods might feel intrusive or overwhelming, leading to further withdrawal from treatment settings. Flexibility and patience are essential components when working with those affected by this disorder.
The Impact of Schizoid PD on Occupational Functioning and Daily Life
Schizoid Personality Disorder significantly affects an individual’s occupational functioning and daily life. Those with this condition often feel detached from social interactions, making it challenging to thrive in team-oriented environments.
Workplaces that emphasize collaboration may present unique challenges for individuals with Schizoid PD. They may prefer solitary tasks and find frequent social engagement draining or overwhelming. This preference can impact job performance and career advancement opportunities.
Daily life can also be affected by a lack of motivation to engage in routine activities or seek fulfilling relationships. Social events, even those intended for leisure, might seem unappealing, leading to further isolation.
The struggle to connect emotionally with others complicates personal relationships as well. Friends and family may misinterpret their behavior as aloofness, exacerbating feelings of loneliness.
Navigating these complexities requires understanding from peers and employers alike.
Comorbidities: Schizoid PD and Other Mental Health Disorders
Comorbidities are common in individuals with Schizoid Personality Disorder (PD). This condition often coexists with other mental health issues, complicating diagnosis and treatment.
Many individuals with schizoid traits might also experience depression or anxiety. These emotional disorders can stem from prolonged social isolation and a lack of fulfilling relationships.
Additionally, some may display features of avoidant personality disorder. The fear of negative evaluation can overlap significantly with the characteristics seen in schizoid PD.
Substance use disorders are another concern. To cope with their feelings of detachment or loneliness, some may turn to alcohol or drugs as a form of self-medication.
Understanding these comorbidities is crucial for developing effective treatment plans. A comprehensive approach that addresses each disorder can lead to better outcomes for those affected by Schizoid Personality Disorder.
Cultural Variations in the Expression and Perception of Schizoid Traits
Cultural context plays a significant role in how schizoid traits are expressed and perceived. In some societies, individuals who prefer solitude may be viewed as introspective or wise. This can lead to a more positive valuation of their behavior.
Conversely, in cultures that emphasize sociability and community involvement, such traits might attract negative attention. People with schizoid characteristics could be labeled as reclusive or antisocial.
The stigma surrounding mental health varies widely across different regions. Some cultures may lack understanding of personality disorders altogether, leading to misconceptions about those with schizoid personality disorder.
Furthermore, cultural expectations shape interpersonal relationships significantly. In collectivist societies, the pressure for social engagement can create internal conflict for individuals exhibiting these tendencies.
Understanding these variations is crucial for mental health professionals working globally. It allows them to tailor approaches based on cultural sensitivities and improve support strategies for affected individuals.
Future Research Directions and Emerging Therapies for Schizoid PD
As we look to the future, research on Schizoid Personality Disorder is poised for exciting developments. The exploration of genetic markers and neurobiological underpinnings could provide deeper insights into its origins and manifestations. Understanding how brain structure influences emotional processing may lead to targeted interventions.
Emerging therapies that focus on enhancing social skills and emotional expression are gaining traction. These approaches aim not only to alleviate symptoms but also to enrich the lives of individuals living with this condition.
Innovative methods, such as virtual reality therapy, might offer new avenues for engagement without overwhelming those who prefer solitude. Furthermore, integrating mindfulness-based practices can help improve self-awareness and acceptance among individuals with Schizoid PD.
Collaboration between researchers, clinicians, and patients will be vital in shaping effective treatment strategies tailored to individual needs. As awareness grows within mental health communities about Schizoid Personality Disorder, so too does hope for those seeking understanding and support in navigating their unique experiences.