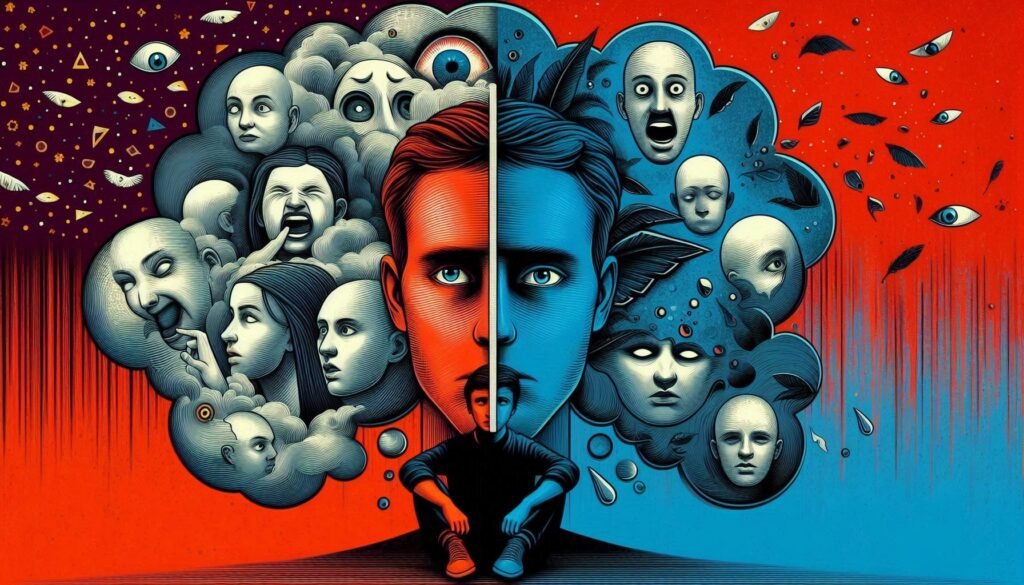
Schizotypal Personality Disorder (STPD) often dances on the fine line between reality and imagination, captivating our curiosity while challenging our understanding of the human mind. Individuals with this complex disorder may appear eccentric or socially withdrawn, yet their unique perspectives offer a glimpse into an intricate world shaped by vivid thoughts and unusual beliefs.
This blog post aims to explore various facets of Schizotypal Personality Disorder—from its defining characteristics to its impact on daily life—shedding light on what it truly means to navigate existence with STPD. Whether you’re seeking knowledge for personal reasons or simply wish to deepen your understanding of mental health, join us as we unravel the layers surrounding Schizotypal Personality Disorder and uncover the truths hidden within its enigmatic nature.

Defining Schizotypal Personality Disorder: Characteristics and Diagnostic Criteria
Schizotypal Personality Disorder is characterized by a pervasive pattern of social and interpersonal deficits. Individuals often experience acute discomfort in close relationships, leading to significant anxiety.
Those with STPD display eccentric behaviors and unusual beliefs. They may have magical thinking or odd speech patterns that set them apart from their peers. Their perceptions can be distorted, contributing to an unconventional worldview.
Diagnostic criteria for Schizotypal PD include at least five specific traits: ideas of reference, odd beliefs or magical thinking, unusual perceptual experiences, suspiciousness, inappropriate emotional responses, and lack of close friends outside family ties.
These symptoms must persist over time and cause functional impairment in personal and professional areas of life. Understanding these characteristics aids in the recognition and management of this complex disorder while fostering empathy toward those affected by it.
Epidemiology of Schizotypal PD: Prevalence Rates and Risk Factors
Schizotypal Personality Disorder (SPD) is estimated to affect approximately 3% of the general population. This prevalence can vary based on geographical and cultural factors, making it essential to consider regional differences when assessing its impact.
Risk factors for developing SPD include a familial history of schizophrenia or related disorders. Genetics plays a crucial role, suggesting that individuals with relatives who have psychotic disorders may be more susceptible.
Environmental influences also contribute significantly. Early childhood trauma, neglect, or adverse life events are known to increase the likelihood of developing schizotypal traits later in life.
Gender differences are observed as well; males tend to exhibit higher rates compared to females. Understanding these epidemiological aspects helps inform targeted interventions and improves awareness within communities about Schizotypal Personality Disorder’s complexities.
The Genetic Basis of Schizotypal Personality Disorder
Research indicates that genetics play a significant role in the development of Schizotypal Personality Disorder (STPD). Family and twin studies suggest a heritable component, with first-degree relatives of those diagnosed exhibiting higher rates of similar traits.
Certain genetic variations may increase vulnerability to STPD. For instance, polymorphisms in genes related to neurotransmitter systems, particularly dopamine and serotonin, have been studied for their potential links to schizotypal features. These genetic factors could influence how individuals process information and perceive reality.
Moreover, ongoing research aims to identify specific gene-environment interactions that contribute to the disorder. Understanding these connections can help clarify why some individuals develop STPD while others do not despite similar environmental exposures. This insight is vital for developing targeted interventions and support strategies tailored to individual needs within this population.
Environmental Influences on the Development of Schizotypal PD
Environmental factors play a significant role in the development of Schizotypal Personality Disorder (PD). Childhood experiences, particularly those involving trauma or neglect, can contribute to the emergence of symptoms. Such early adverse events may disrupt normal emotional and social development.
Family dynamics also matter. Growing up in an environment with high levels of conflict or instability can increase vulnerability to developing schizotypal traits. A lack of supportive relationships further exacerbates these risks.
Cultural context influences how individuals express schizotypal characteristics. In some cultures, eccentric behaviors might be celebrated rather than stigmatized, affecting diagnosis and treatment approaches.
Additionally, peer interactions during formative years shape social cognition skills. Negative peer experiences can heighten feelings of isolation and reinforce maladaptive coping strategies commonly seen in those with Schizotypal PD.
Neurocognitive Profiles in Schizotypal Personality Disorder
Individuals with Schizotypal Personality Disorder (SPD) often exhibit distinct neurocognitive profiles. Research indicates that they may struggle with attention, working memory, and executive functioning. These cognitive challenges can manifest as difficulties in organizing thoughts or managing tasks.
Studies suggest that abnormalities in brain regions involved in these functions contribute to the symptoms of SPD. For instance, the prefrontal cortex and temporal lobes are often implicated. Dysfunction in these areas can lead to impaired reasoning and social cognition.
These cognitive deficits might also explain some of the eccentric behaviors associated with SPD. Individuals may engage in unique thought processes or display unusual beliefs, which can complicate their interactions with others.
Understanding these neurocognitive aspects is crucial for developing effective treatment strategies tailored to address specific needs within this population. This approach fosters a more comprehensive perspective on Schizotypal Personality Disorder and its impact on daily functioning.
Perceptual Aberrations and Magical Thinking in Schizotypal PD
Individuals with Schizotypal Personality Disorder often experience perceptual aberrations. These can manifest as altered sensory perceptions, including heightened sensitivity to sounds or visual distortions. Such experiences may lead to a distorted sense of reality.
Magical thinking is another hallmark of this disorder. People might believe that their thoughts can influence events in the external world. For instance, they may think wishing for something could make it happen. This form of cognition often blurs the lines between imagination and reality.
These traits contribute to unique worldviews that set individuals apart from societal norms. They might find solace in unconventional beliefs or rituals, creating a personal framework for understanding life’s complexities.
While these characteristics can be intriguing, they also pose challenges in daily functioning and relationships. Understanding them is essential for effective support and intervention strategies tailored to those affected by Schizotypal PD.
Social Cognition and Interpersonal Difficulties in Schizotypal Individuals
Individuals with Schizotypal Personality Disorder often experience significant challenges in social cognition. This can lead to misunderstandings and misinterpretations of social cues.
Their unique thought processes may cause them to perceive benign interactions as suspicious or threatening. This heightened sensitivity can create barriers in forming and maintaining relationships.
Moreover, the tendency toward eccentric behaviors may alienate others, further complicating social dynamics. Many individuals find it difficult to engage in typical conversational exchanges, leading to awkwardness and isolation.
These interpersonal difficulties are amplified by a lack of trust in others. Consequently, building meaningful connections becomes increasingly challenging for those affected by this disorder.
Understanding these nuances is crucial for both individuals with Schizotypal traits and those around them, fostering empathy and patience in social situations.
The Relationship Between Schizotypal PD and Schizophrenia Spectrum Disorders
Schizotypal Personality Disorder (SPD) shares certain features with schizophrenia spectrum disorders, yet they remain distinct diagnoses. Individuals with SPD may exhibit odd beliefs and eccentric behaviors, which can sometimes mimic the early symptoms of schizophrenia.
Research indicates that both conditions involve disruptions in thought processes. However, those with schizotypal traits generally maintain a grasp on reality. They often do not experience hallucinations or delusions as prominently as individuals diagnosed with schizophrenia.
Genetic studies also suggest overlapping hereditary factors between SPD and schizophrenia spectrum disorders. This genetic connection highlights similarities in brain structure and function that warrant further exploration.
Understanding these relationships is vital for accurate diagnosis and effective treatment options. Clinicians must differentiate between the two to ensure patients receive appropriate mental health support tailored to their unique needs.
Assessment Tools and Diagnostic Challenges in Schizotypal PD
Assessment of Schizotypal Personality Disorder (PD) requires a nuanced approach. Clinicians often rely on structured interviews and standardized questionnaires to gather information about an individual’s thoughts, behaviors, and relationships.
Tools like the Structured Clinical Interview for DSM-5 (SCID-5) help identify core symptoms such as eccentric behavior or perceptual distortions. However, diagnosing Schizotypal PD can be challenging due to symptom overlap with other personality disorders and mental health conditions.
Moreover, self-report instruments may not capture the full extent of the disorder. Individuals might struggle to recognize their odd beliefs or social anxieties, complicating accurate diagnosis.
Cultural factors also play a role in assessment. Variations in expression of symptoms across different cultures can lead to misinterpretation by clinicians unfamiliar with these nuances. Thus, thorough exploration is essential for effective identification and understanding of this complex disorder.
Evidence-Based Psychotherapeutic Approaches for Schizotypal Personality Disorder
Psychotherapeutic approaches for Schizotypal Personality Disorder (SPD) focus on enhancing social skills and reducing anxiety. Cognitive Behavioral Therapy (CBT) is a prominent method, targeting distorted thinking patterns. This can help individuals challenge irrational beliefs and improve their emotional responses.
Schema therapy also plays a vital role. It aims to identify negative life patterns formed in childhood, promoting healthier coping mechanisms. By addressing these maladaptive schemas, patients can foster better self-esteem and interpersonal relationships.
Group therapy offers another dimension of treatment. Interacting with peers helps build social confidence and reduces feelings of isolation. Sharing experiences within a supportive environment validates individual struggles while encouraging personal growth.
Mindfulness-based therapies are gaining traction too. These techniques assist individuals in staying present, reducing stress levels associated with their symptoms.
Each approach addresses specific challenges that those with SPD face, paving the way for improved functioning in daily life.
Pharmacological Interventions in the Treatment of Schizotypal PD
Pharmacological interventions for Schizotypal Personality Disorder (PD) primarily focus on alleviating specific symptoms rather than treating the disorder as a whole. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are commonly prescribed to address mood instability and anxiety often experienced by individuals with this condition.
Antipsychotic medications may also play a role in managing cognitive distortions or perceptual abnormalities that some patients encounter. Low doses of atypical antipsychotics can help reduce these symptoms while minimizing side effects.
Despite their potential benefits, there is limited research specifically targeting pharmacotherapy for Schizotypal PD. As such, treatment plans should be tailored to each individual’s needs, balancing medication use with therapeutic approaches like psychotherapy. Regular monitoring is vital to assess efficacy and adjust prescriptions accordingly.
Collaboration between healthcare providers and patients fosters an effective framework for managing Schizotypal Personality Disorder through pharmacological means.
The Impact of Schizotypal PD on Quality of Life and Functioning
Schizotypal Personality Disorder profoundly influences an individual’s quality of life and daily functioning. Those affected often experience significant social anxiety, leading to difficulties in forming and maintaining relationships.
Their unconventional beliefs and eccentric behaviors can alienate them from peers. This isolation exacerbates feelings of loneliness, creating a cycle that further impacts their mental well-being.
Occupational functioning may also suffer due to erratic thought patterns or misunderstandings with colleagues. Individuals might struggle with workplace dynamics, making it challenging to achieve career goals.
Moreover, the emotional distress associated with Schizotypal PD can hinder personal growth. Coping mechanisms might include avoidance strategies rather than proactive engagement in therapy or support systems.
The interplay between these factors contributes to a diminished sense of self-worth and overall life satisfaction for those living with this disorder. Understanding these challenges is crucial for providing effective support and interventions that enhance their quality of life.
Cultural Considerations in the Expression and Diagnosis of Schizotypal Traits
Cultural context plays a significant role in how schizotypal traits are expressed and perceived. Different cultures have distinct beliefs, values, and social norms that can shape behaviors and thought patterns associated with Schizotypal Personality Disorder.
For instance, what may be considered eccentric or unusual in one society might be viewed as normal within another cultural framework. This variability complicates the diagnostic process, as clinicians must navigate these differences to avoid misdiagnosis.
Additionally, stigma surrounding mental health varies greatly across cultures. In some societies, individuals exhibiting schizotypal characteristics may face ostracism rather than receive appropriate support and care.
Understanding cultural nuances is crucial for accurate diagnosis and effective treatment of schizotypal traits. Clinicians should remain culturally aware to provide tailored interventions that respect individual backgrounds while addressing their unique challenges.
Comorbidities: Schizotypal PD and Other Mental Health Conditions
Schizotypal Personality Disorder often coexists with other mental health conditions. This overlap can complicate diagnosis and treatment.
Individuals with Schizotypal PD frequently experience anxiety disorders. Social anxiety is particularly common, as their social interactions can be challenging due to eccentric behavior and distorted perceptions.
Depressive disorders are also prevalent among those diagnosed with Schizotypal PD. Feelings of loneliness and isolation may contribute to depressive symptoms, exacerbating their condition.
Additionally, substance use disorders can arise in this population. Individuals might turn to alcohol or drugs as a coping mechanism for managing distressing thoughts or emotions.
Bipolar disorder has been documented alongside Schizotypal PD in some cases. The interplay between mood fluctuations and personality traits requires careful assessment by mental health professionals.
Recognizing these comorbidities is crucial for effective treatment planning. Tailored interventions should address the complexities presented by overlapping diagnoses to improve outcomes for individuals affected by both conditions.
Future Directions in Research and Treatment of Schizotypal Personality Disorder
The landscape of research and treatment for Schizotypal Personality Disorder (STPD) is evolving rapidly. As mental health professionals gain a deeper understanding of this complex condition, future studies are expected to focus on several key areas.
First, there is an increasing need for longitudinal studies that track individuals with STPD over time. Such research could shed light on the natural progression of the disorder and inform best practices in intervention strategies. Understanding how symptoms evolve can help clinicians tailor their approaches more effectively.
Second, integrating neuroimaging techniques will likely play a significant role in advancing our knowledge about STPD. By examining brain structure and function, researchers may identify specific biomarkers associated with the disorder. This could lead to more accurate diagnoses and targeted treatments based on individual neural profiles.
Additionally, exploration into culturally sensitive frameworks for diagnosing and treating STPD is essential. Mental health practitioners must recognize that cultural backgrounds influence symptom expression and perceptions of reality. Future research should prioritize diverse populations to ensure inclusive care pathways.
On the therapeutic front, ongoing development of evidence-based psychotherapeutic interventions remains crucial. Researchers are examining various modalities such as cognitive-behavioral therapy (CBT), dialectical behavior therapy (DBT), and mindfulness-based approaches tailored specifically for those with STPD traits.
Pharmacological advancements also hold promise in managing symptoms associated with Schizotypal PD. New medications targeting underlying neurobiological processes may enhance existing treatment options or provide alternatives where current therapies fall short.
Fostering collaboration between researchers, clinicians, patients, and families will be vital in driving comprehensive care solutions forward. Engaging all stakeholders creates a holistic approach that addresses both clinical needs and personal experiences related to living with STPD.
As we look ahead at these potential developments within the realm of Schizotypal Personality Disorder research and treatment initiatives stand poised to significantly improve understanding—and ultimately life quality—for individuals affected by this often-misunderstood condition.