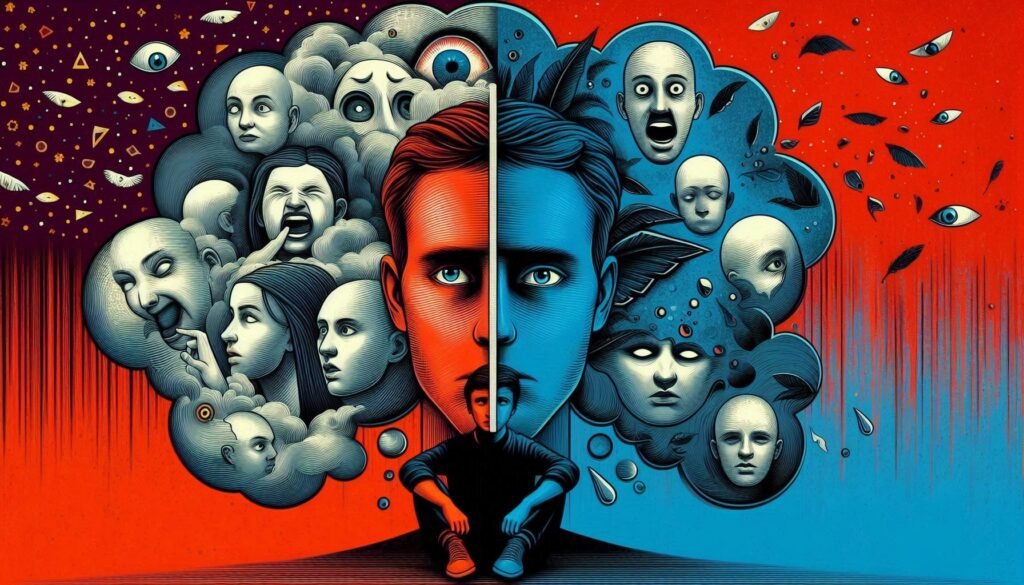
Stress affects everyone, but its expression can vary dramatically from one individual to another. For those with Schizoid Personality Disorder (SPD), stress response patterns take on unique dimensions that intertwine deeply with their core characteristics. Understanding these patterns is essential for offering appropriate support and interventions.
Individuals with SPD often exhibit emotional detachment, which shapes how they experience and manage stress. This blog post aims to unravel the complex interplay between SPD and stress responses. By exploring the neurobiology of stress, cognitive perceptions, physiological reactions, and coping mechanisms in these individuals, we will shed light on a topic that remains both fascinating and crucial for mental health awareness. Whether you’re a mental health professional or simply someone looking to deepen your understanding of SPD, this exploration offers valuable insights into the intricate world of stress response in those who navigate life through a different lens.

Understanding Schizoid Personality Disorder (SPD): Core Features and Diagnosis
Schizoid Personality Disorder (SPD) is characterized by a pervasive pattern of detachment from social relationships and a restricted range of emotional expression. Individuals with SPD often appear indifferent to social norms and engage minimally in close relationships, including family ties.
These individuals typically prefer solitary activities over group interactions. Their interests may revolve around intellectual pursuits rather than social engagement. This can lead to perceptions of aloofness or disinterest from others.
Diagnosis usually involves a thorough clinical assessment, which takes into account the individual’s history and current functioning. Mental health professionals rely on criteria outlined in the DSM-5 for accurate diagnosis, ensuring that other conditions are ruled out first.
Awareness of these core features is crucial for understanding how SPD shapes an individual’s experience, particularly regarding stress response patterns unique to this personality disorder.
The Neurobiology of Stress: General Mechanisms and Pathways
Stress triggers a complex neurobiological response in the body. Central to this process is the hypothalamic-pituitary-adrenal (HPA) axis. When faced with stress, this system activates, releasing hormones such as cortisol.
Cortisol plays a crucial role in managing energy and regulating various bodily functions during stressful situations. It helps mobilize glucose for immediate energy needs while suppressing non-essential processes like digestion or immune function.
Additionally, neurotransmitters such as adrenaline surge through the body, preparing individuals for fight-or-flight responses. This cascade of hormonal changes can affect brain regions like the amygdala, which processes emotions and fear.
The body also experiences physiological effects including increased heart rate and blood pressure. These reactions are part of an adaptive mechanism designed to enhance survival under threat but can become problematic when chronic stress persists over time.
Unique Characteristics of Stress Perception in Schizoid Personality Disorder (SPD) Individuals
Individuals with Schizoid Personality Disorder (SPD) exhibit distinct characteristics in how they perceive stress. Their emotional detachment often leads to reduced awareness of internal feelings and external stimuli. This can result in a muted response to stressful situations, making it difficult for them to recognize when they are under pressure.
Moreover, their preference for solitude may shield them from many stressors that affect others. However, this isolation can also lead to an accumulation of unprocessed stress, which might manifest unexpectedly later on.
Schizoid individuals typically prioritize rational thought over emotional reactions. Consequently, they may interpret stressful events through a logical lens rather than feeling overwhelmed by anxiety or fear. This cognitive style influences their coping mechanisms and overall approach to life’s challenges. Understanding these unique perceptions is crucial for developing effective strategies tailored specifically for SPD individuals facing stress.
Emotional Detachment and Its Impact on Stress Processing
Emotional detachment is a key characteristic of individuals with Schizoid Personality Disorder (SPD). This trait often leads to an altered experience of stress. People with SPD tend to avoid emotional engagement, which can make it challenging for them to process stress effectively.
When under pressure, their lack of emotional expression may mask underlying feelings. They might not exhibit typical signs of distress, leading others to underestimate the severity of their situation.
This detachment can serve as a protective barrier, but it also limits their ability to seek support from others. Without external validation or assistance, coping mechanisms may become less effective over time.
As a result, unresolved stressors can accumulate internally. The inability or unwillingness to confront emotions could lead to increased tension and potential health issues in the long run. Understanding this dynamic is crucial for developing tailored therapeutic interventions that address these unique challenges faced by those with SPD.
Physiological Stress Responses in Schizoid Personality Disorder (SPD)
Individuals with Schizoid Personality Disorder (SPD) often exhibit distinct physiological stress responses. While they may appear detached, their bodies still react to stress in unique ways.
Research indicates that individuals with SPD might have an altered hypothalamic-pituitary-adrenal (HPA) axis response. This can lead to atypical cortisol levels during stressful situations. Elevated or diminished cortisol production may affect mood and energy levels.
Moreover, heart rate variability can differ significantly in those with SPD. They might show a reduced capacity for autonomic regulation under stress, impacting both emotional and physical well-being.
Interestingly, the lack of external expression doesn’t mean these individuals are immune to physical symptoms. Many report somatic complaints like headaches or gastrointestinal issues when stressed, reflecting internalized tension rather than outward signs of distress. Understanding these physiological nuances is crucial for tailored interventions and support strategies for those navigating SPD challenges.
Cognitive Patterns in SPD: Influence on Stress Interpretation
Cognitive patterns in individuals with Schizoid Personality Disorder (SPD) significantly shape their interpretation of stress. These individuals often exhibit a distinctive way of processing information, which can skew their perception of stressful situations.
Many with SPD prefer solitude and distance from emotional stimuli. This detachment influences how they assess challenges or threats. They may downplay the severity of stressors or perceive them as irrelevant, leading to an atypical response.
Additionally, cognitive rigidity is common among those with SPD. Their fixed thought patterns make it difficult to adapt when faced with new stresses. This inflexibility can result in increased anxiety if unexpected changes occur.
Moreover, these cognitive styles contribute to a tendency toward introspection rather than external engagement. While this self-focus might seem beneficial at times, it can inhibit effective problem-solving during stressful periods, leaving them feeling overwhelmed without clear coping strategies available.
Social Withdrawal as a Stress Management Strategy in SPD
Social withdrawal is a common response for individuals with Schizoid Personality Disorder (SPD) when faced with stress. This behavior acts as a protective shield against overwhelming emotions and external pressures.
By retreating into solitude, SPD individuals often feel a sense of control. They can avoid the anxiety that social interactions may provoke. This isolation provides them time to process their thoughts without interference.
However, while this strategy may offer temporary relief, it can exacerbate feelings of loneliness and emotional detachment in the long run. The lack of social engagement prevents healthy coping mechanisms from developing.
Additionally, repeated withdrawal can lead to missed opportunities for connection and support. As they isolate themselves further, building trust and relationships becomes increasingly challenging.
Understanding these dynamics is crucial for addressing stress management in people with SPD effectively. Social strategies need careful consideration to help navigate their unique experiences with stress.
The Role of Alexithymia in Stress Experiences of SPD Individuals
Alexithymia, characterized by difficulties in identifying and expressing emotions, plays a significant role in the stress experiences of individuals with Schizoid Personality Disorder (SPD). This emotional disconnect can hinder their ability to recognize stressors effectively.
Without a clear understanding of their feelings, SPD individuals may struggle to respond appropriately to stressful situations. They might remain unaware of the physiological signs that often accompany stress, such as increased heart rate or muscle tension.
This inability to articulate emotions can lead to heightened levels of anxiety and frustration. When faced with stress, they may retreat further into isolation rather than seeking help or engaging in coping strategies.
Consequently, this pattern not only intensifies their emotional detachment but also complicates their overall mental health journey. Understanding this connection between alexithymia and stress is crucial for developing effective therapeutic approaches tailored for those with SPD.
Comorbidity: How Other Disorders Affect Stress Responses in SPD
Comorbidity plays a significant role in shaping stress response patterns in individuals with Schizoid Personality Disorder (SPD). Many people with SPD may experience additional mental health conditions, such as depression or anxiety disorders. These overlapping issues can complicate how stress is perceived and managed.
For instance, the presence of anxiety might heighten sensitivity to everyday stressors. An individual already struggling with emotional detachment may find it challenging to cope effectively when faced with increased pressure.
Moreover, depressive symptoms can lead to withdrawal from social interactions that would typically provide support during stressful times. This isolation further exacerbates feelings of helplessness and increases distress.
Understanding these dynamics is crucial for developing effective treatment strategies that address both SPD and its comorbid conditions. Tailored therapies can help individuals navigate their complex emotional landscapes while improving their overall resilience against stress.
Assessment Tools for Measuring Stress in Schizoid Personality Disorder
Measuring stress in individuals with Schizoid Personality Disorder (SPD) requires tailored assessment tools. Traditional stress measurement scales may not capture the unique emotional landscape of those with SPD.
One effective tool is the Stress Vulnerability Questionnaire, which evaluates personal and environmental factors influencing stress responses. This instrument focuses on individual experiences rather than societal norms.
The Alexithymia Scale can also be beneficial. It assesses an individual’s ability to identify and express emotions, shedding light on how emotional detachment affects their perception of stress.
Additionally, qualitative interviews provide deep insights into personal narratives surrounding stress. They help clinicians understand specific triggers and coping mechanisms employed by individuals with SPD.
Combining quantitative assessments with qualitative approaches offers a comprehensive view of how SPD influences stress response patterns, allowing for more accurate diagnoses and targeted interventions.
Therapeutic Approaches to Enhancing Stress Management in Schizoid Personality Disorder (SPD)
Therapeutic approaches for individuals with Schizoid Personality Disorder (SPD) aim to enhance stress management through tailored interventions. One effective method is cognitive-behavioral therapy (CBT), which helps modify negative thought patterns and improve emotional awareness.
Mindfulness techniques also play a crucial role in managing stress. These practices encourage present-moment focus, helping individuals reconnect with their emotions and sensations without judgment. This can be particularly beneficial for those who often feel detached.
Group therapy can provide a supportive environment where SPD individuals learn from others’ experiences. It fosters social skills development while reducing feelings of isolation.
Additionally, art or music therapy offers non-verbal outlets for expression. Creative therapies allow exploration of emotions in a safe space, making it easier to process stressors constructively.
These varied therapeutic modalities empower individuals with SPD to better understand their unique responses and develop healthier coping strategies over time.
The Impact of Chronic Stress on SPD Symptom Progression
Chronic stress can significantly exacerbate symptoms in individuals with Schizoid Personality Disorder (SPD). When under prolonged stress, the emotional detachment characteristic of SPD may deepen. This can lead to further isolation and difficulty connecting with others.
Stress impacts neurotransmitter balance in the brain, potentially worsening mood regulation issues common to those with SPD. As these chemical changes occur, existing symptoms like withdrawal and indifference can intensify.
Moreover, chronic stress affects cognitive functions. Individuals might find it harder to process emotions or even recognize them in themselves, complicating their daily interactions. This disconnection from feelings makes managing relationships increasingly challenging.
Furthermore, chronic stress may manifest physically as fatigue or somatic complaints. These physical symptoms often compound psychological challenges, creating a cycle that is difficult to break for those living with SPD.
Coping Mechanisms: Adaptive and Maladaptive Strategies in SPD
Individuals with Schizoid Personality Disorder (SPD) often navigate their world using specific coping mechanisms. These strategies can be categorized as adaptive or maladaptive, influencing how they handle stress.
Adaptive strategies might include solitary activities that provide comfort and relaxation. Engaging in hobbies like reading or artistic pursuits allows for self-expression while minimizing interaction with others. Such methods foster a sense of control and emotional regulation.
On the other hand, maladaptive strategies may surface when individuals withdraw excessively from social situations. This avoidance can enhance feelings of loneliness and exacerbate symptoms of SPD over time. Additionally, some may resort to intellectualization, distancing themselves emotionally from stressors instead of addressing underlying issues.
Understanding these coping mechanisms is crucial for developing effective therapeutic interventions tailored to the unique needs of those with SPD. Balanced approaches can promote healthier responses to stress while enhancing overall well-being.
Interpersonal Relationships and Stress Dynamics in Schizoid Individuals
Interpersonal relationships play a crucial role in shaping stress dynamics for individuals with Schizoid Personality Disorder (SPD). Due to the core features of SPD, such as emotional detachment and social withdrawal, these individuals often experience unique challenges in their interactions. Their tendency to avoid close relationships can lead to feelings of isolation, which may exacerbate stress levels.
Moreover, their difficulty connecting emotionally can create misunderstandings with others. Friends or family members might misinterpret their aloofness as disinterest or indifference. This misunderstanding can further strain bonds and leave SPD individuals feeling unsupported during stressful times.
It’s important to recognize that while they may seem indifferent on the surface, those with SPD still have internal experiences of stress that are not always visible. The lack of social support systems makes it essential for them to develop stronger coping mechanisms tailored for interpersonal settings.
Therapeutic interventions focusing on enhancing communication skills and providing safe spaces for emotional expression can be beneficial. Understanding how stress affects relational dynamics empowers both the individual and those around them towards fostering healthier connections. Adjusting expectations in relationships could lessen pressure and promote more meaningful interactions despite the inherent challenges posed by SPD characteristics.
Improving interpersonal dynamics not only aids in better managing stress but also facilitates a deeper understanding between individuals with SPD and those who care about them—ultimately leading toward improved well-being.